Pelvic Therapy and Gynecological Cancer
This is a subtitle for your new post
When someone hears the diagnosis of cancer, the medical model immediately presents your treatment options and prognosis. Each patient is different, but we can imagine the brain goes “fight or flight” and pushes through whatever treatment is needed in order to beat the cancer. Often, very little thought is given to “life after cancer.”
What symptoms will I have?
Will I have to get treatment for symptoms caused by my cancer treatment?
When will this end?
Will I ever be “normal” again?
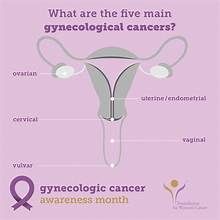
These questions are valid, and you may not have someone on your healthcare team who is readily available to answer them. They can be difficult to ask, especially in women who have survived
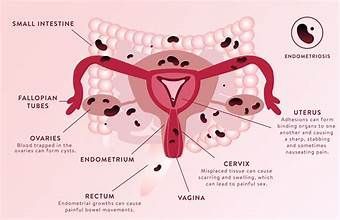
gynecological cancers,
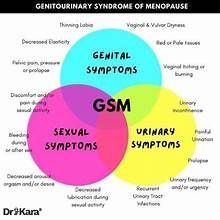
or cancer of the uterus, ovaries, breast, or cervix. Some of the biggest complaints following treatment of GYN cancers include pelvic pain, painful sex, urinary urgency and urinary leakage. Imagine just finishing your chemotherapy or radiation and then having to deal with that!
A recent study followed 31 women who had finished their cancer treatment at least three months prior. They were cancer free, but were complaining of painful sex, decreased sexual desire and urinary symptoms. The participants attended 12 visits of pelvic floor physical therapy, one visit per week. The study states,
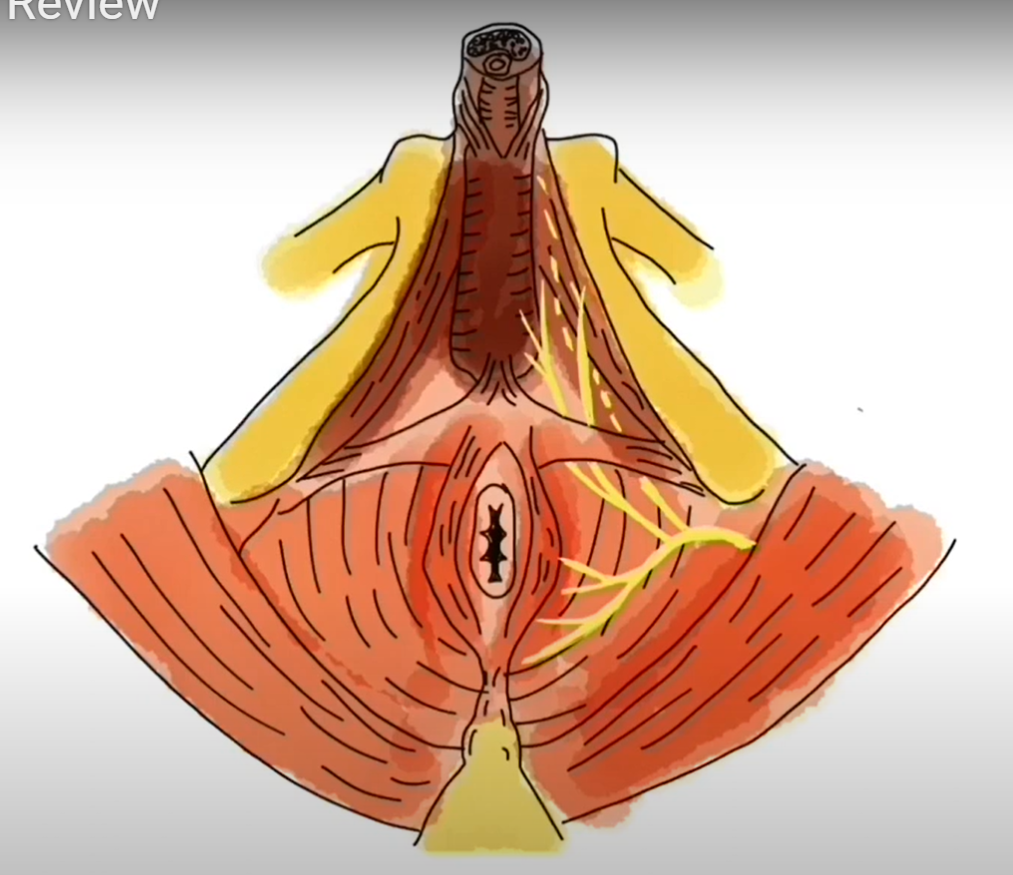
“At each session, the physical therapist provided information, advice and support to women. She explained the underlying mechanisms of chronic pain experienced during sexual intercourse after gynecological cancer including the role of the pelvic floor muscles and how the treatment could help to reduce the pain. She gave additional information about how to manage chronic pain and other pelvic floor disorder symptoms (e.g., bladder training). The use of relaxation techniques using deep breathing as well as the application of vaginal lubricants and moisturizers were encouraged. The physical therapist also helped the participants gain more knowledge about sexual functioning (i.e., physiology of desire, excitation and orgasm) and guided them into resuming non-painful sexual activities with their partners.”
They continued,
“At each session, manual therapy techniques (i.e., stretching, myofascial release and tissue desensitization) and pelvic floor muscle exercises with electromyography biofeedback (i.e., relaxation, motor control, strength and endurance) using a small intra-vaginal probe were used. Women were also asked to perform home exercises resembling those performed under supervision five times per week as well as auto-insertion exercises with a finger or graded vaginal dilator in addition to desensitization techniques three times per week.”
In a nutshell, the PTs used biofeedback, muscle stretching, relaxation and breathing exercises, vaginal dilators, and lots of education during their treatment sessions. The combination of these interventions would look different depending on the patient but, to an extent, all would be used.
Did it work?
This is a table showing what the participants reported. The left column describes their report in terms of how their physical bodies felt, and the right lists improvements in psychological health.
We would say
absolutely yes, physical therapy helped significantly!
The authors stated “All participants reported experiencing less pain during intercourse, with several stating having no pain at all since the end of the PFPT........the vast majority mentioned their vagina being less dry and more naturally lubricated during sexual activities. Among other things, several women emphasized not needing to use vaginal products anymore and reported being less stressed and more interested in engaging in sexual activities.”
Some participants stated:
“All the exercises [contraction and stretching] I had done and what the physical therapist had done removed the tension and loosened me up. It felt good. Penetration was easier.” –C01
“It helped me to understand how my body reacted to a lot of things, to understand that I was not alone and it helped me to accept myself and accept living my sex life in a different way. It [the treatment] allowed us to make different connections. There is a lot, really a lot of affection. It starts slowly, and, in the end, it becomes intense. This is what is new, this is what we learned.” –C17B
Half of the participants experienced either stress urinary incontinence, urgency urinary incontinence or symptoms of urinary urgency before the study.
All women reported significant improvements following PFPT.
Another participant stated:
“All the exercises, the squeezing and all that helped. You squeeze and it calms your bladder. I didn’t think it would work. Listen, I can even hold my urine when I go to the bathroom. . . Before, when I saw the toilet, I had to run and when I saw the toilet bowl, I leaked two or three drops. But now, I am able to hold it. I know what to do.” –C10
Entering cancer treatment can be very scary. It can alter our sense of self. One of the study participants described it perfectly,
“After cancer treatments, you feel diminished. Will it come back as before? I was starting to be afraid. With physical therapy, you feel less diminished. It seemed as if it was finally possible that things could get better. When I got into the program, it was another story as I realized it was possible to improve, and it was much less upsetting, less scary. It’s because we found where it hurt most. It’s about understanding. . . It’s partly confidence, partly the fear that’s gone.”–C124
If you have pelvic floor symptoms of any kind following your cancer treatment, know there is a team waiting to help you.