Chronic Pelvic Pain
This is a subtitle for your new post
We’ve all heard of asthma, right? This respiratory condition affects 8% of Americans, and almost everyone knows someone who has it.¹ Depending on the type of asthma, it can lead to a significant decrease in activity tolerance and overall quality of life. Although asthma is important and affects a lot of people, it doesn’t have much to do with pelvic health. So why are we talking about it?
Pelvic pain is similar to asthma in that depending on the type, it can cause a very significant shift in your ability to perform daily responsibilities and decrease quality of life. The prevalence of pelvic pain
doubles that of asthma.
One study noted 25% of women experience this at some point in their lives, and another reports 8% prevalence in men.² ³
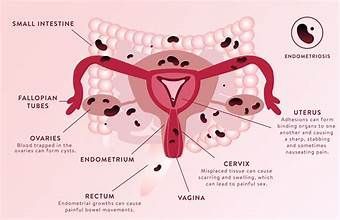
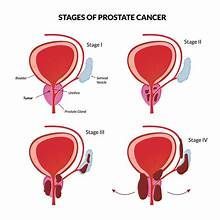
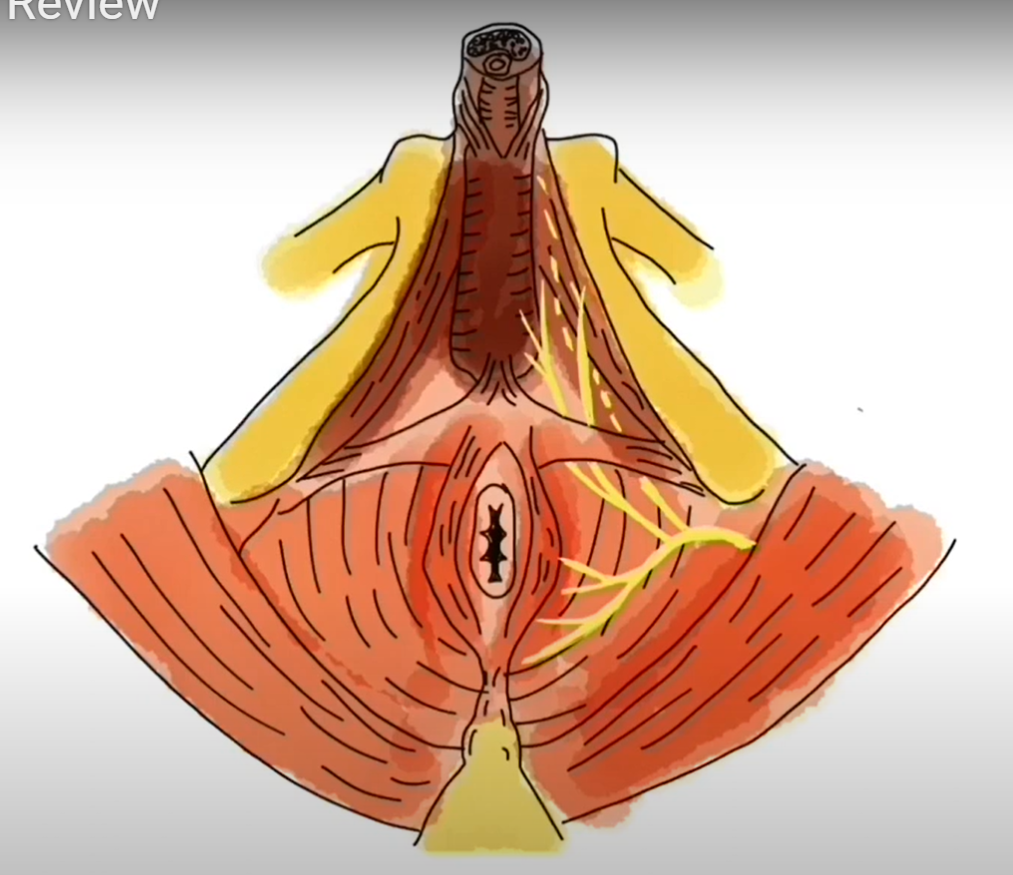
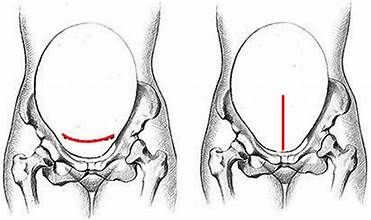
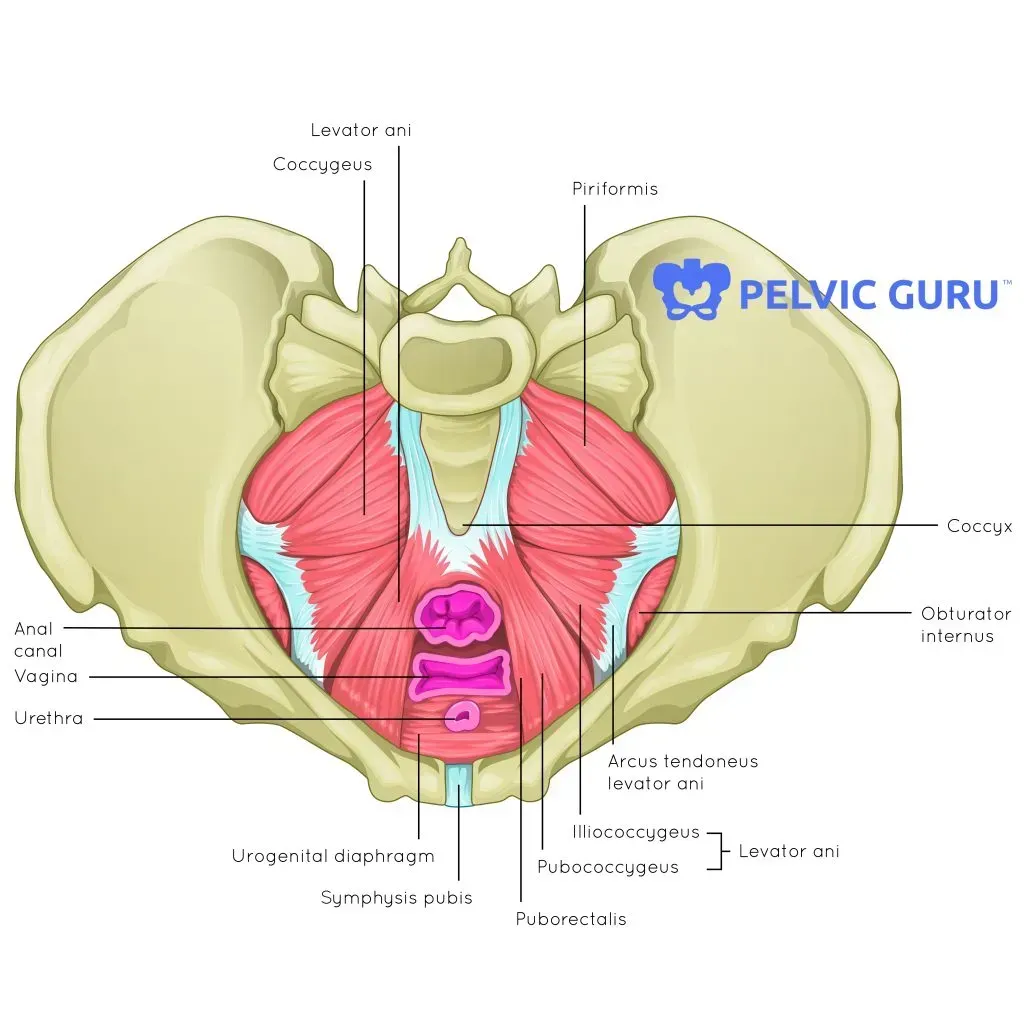
Your pelvis begins just below your belly button, and ends at the bottom of the gluteal folds (just below your gluteal muscles). Within this area of the body we have all kinds of muscles, bones, nerves, arteries, and organs that could potentially contribute to pain - uterus and ovaries, bladder, colon, sacroiliac joint, abdominal muscles, prostate, sciatic nerve, just to name a few. You can see in the pictures below just how involved the pelvis really is!
Dysfunction in any of the structures within the pelvis can cause pain, which can make diagnosing the core of the problem difficult. Often, we see clients who have had this pelvic pain for years, seen a multitude of providers, tried every treatment option in the book, to no avail. It can be extremely troubling, disheartening, and defeating to have constant pain with no answer as to where it’s coming from.
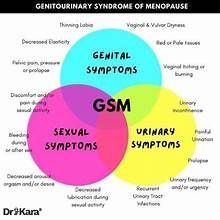
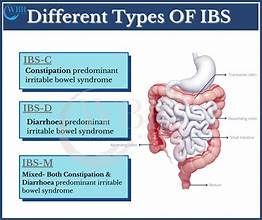
So, what causes pelvic pain? According to a paper written by Dr. Fred Howard in 2011, the leading causes of pelvic pain in women include pelvic nerve neuralgia, myofascial pain and trigger points, Irritable Bowel Syndrome, Interstitial Cystitis, and endometriosis.4
We will talk in detail about myofascial (muscle) pain and trigger points later in this post.
See the link in reference list for the complete list of diagnoses and their definitions. If you have ever been diagnosed with any one of these, it is likely that you’re experiencing pelvic pain. That does not mean that if you haven’t received a diagnosis like the ones listed above, that you don’t have pelvic pain. If you are having pain in the pelvic area at all, that warrants seeking help!
When clients come in with a main complaint of pelvic pain, we often hear them report the same kinds of things. Some of the most common reports include:
- “I have pain in my buttock and around my vaginal area if I sit for longer than 30 minutes.”
- “Sex is okay, but sometimes it feels like my partner is hitting a bruise when we try certain positions.”
- “My periods have always been really heavy and painful, and I’ve never been able to insert a tampon without pain.”
- “My doctor diagnosed me with chronic prostatitis and I’ve had the surgery, but my pain never went away.”
- “I have constant pain in my abdomen, and I’ve noticed it gets worse when I eat my favorite spicy meal or drink a Diet Coke.”
- “I’ve struggled with constipation for years, and lately it’s started to hurt when I have bowel movements.”
- I’m waking up 5 or 6 times a night to go to the bathroom. It feel like I have the urge to go all day long!”
Have you ever said or thought these things? Have you tried antibiotics, elimination diets, MRI and x rays, injections, and more to get rid of that nagging pain between your belly and your bum? Or maybe you have just started experiencing this type of pain and have chalked it up to the aging process and don’t plan on seeking help. Whatever your personal history may be, pelvic pain is common but never normal. Pelvic health physical therapy is one option that you may have never heard of, but that offers relief to so many people!
The great thing about seeing a
pelvic health PT is that you can almost guarantee we’ve heard all of your symptoms before, and have treated hundreds of other people just like you. If you’ve read any of the previous blogs on this page, you’re familiar with the set of muscles at the bottom of your pelvis, so rightly named the “pelvic floor muscles (PFM)”. In patients with pelvic pain these muscles are often too tight and are holding tension.
Picture this: you just had the most stressful day at work. The to-do list is longer than ever, your cubicle neighbor is getting on your nerves, and you and your boss get into a disagreement. You finally head home at the end of the day only to be greeted with a sink full of dirty dishes, two kids waiting on dinner to be cooked, and the house has to be cleaned for the dinner party you’re hosting tomorrow night. Not to mention you have a work deadline, due tomorrow. Sound familiar? Maybe this doesn’t describe your current season of life, but we all know the feeling of being stressed and feeling like there just isn’t enough time in the day. When we become stressed, our body reacts and we get tense. We’ve all had those days when we get home and it feels like our shoulders are up to our ears and we just can’t seem to relax. Oddly enough, that small group of PFM that we can’t even see (and often ignore) can carry tension in the same way our shoulder and neck muscles do. When these muscles stay in a tensed, contracted state for long periods of time, they can forget how to relax. When that happens less blood flow is delivered to the muscles, they aren’t able to get the oxygen and nutrients they need, and you begin to experience pain. We don’t always know why our PFM tense up and stay there, but there are some risk factors that can lead to an overactive pelvic floor: stress, pregnancy and delivery, pelvic surgery, and/or sexual abuse.5 Up to 25% of all women have experienced some type of sexual abuse, which often has implications for pelvic, and overall, health. In one study 17% of the women who visited an OBGYN clinic reported sexual abuse in their past, and in the study analysis chronic pelvic pain was significantly associated with a history of abuse .6
Regardless of cause, these muscles need to learn how to release, relax, and let go of the tension they’ve been holding on to, but this can be harder than it sounds. A pelvic floor physical therapist is an expert at assessing whether or not your PFM are too tight, and deciding which treatment options are best suited for you. Here are some things a pelvic floor PT may do to help with your pelvic pain:
- Assess your posture - our PFM work best when we are in a neutral posture and our core is most stable. Your PT can teach you how to find that posture and how to maintain it.
- Assess your leg, abdominal, and gluteal muscles - sometimes the muscles surrounding your pelvis get too tense and irritable as well. Your therapist can massage these tense spots out, resulting in a decrease in pain.
- Teach you to breath - sounds easy, right? Well, not always. Your posture and breath are intimately related, as are your breathing diaphragm and the PFM. With a good foundation in place for breathing, it can make relaxation a much easier task.
- Relaxing - your therapist can give you tips and tricks on how to implement relaxation and stress relief into your daily routine, and make sure that your bones and muscles are in the right “state of mind” to aid that relaxation.
- Assess your PFM - Pelvic health PTs have the unique ability to assess your muscles on the inside of your pelvis, similar to a routine pelvic exam (minus the stirrups and speculums). This is one of the best ways to get to the root of your pain, and decide if the muscles are too tensed. If you are having pain and an internal exam seems out of the question for you, there are plenty of other ways to help. See the “FAQs” blog post for more detail about the internal muscle assessment.
- Massage and stretching for the PFM - your therapist is able to access these muscles and find “trigger points” that can contribute to pain. With very gentle pressure and light stretching to these muscles, your trigger points can be resolved and blood flow restored to the muscles, giving them the ability to fully relax again.
- Other stretches and exercise programs - when people think of pelvic health PT they mostly think of Kegels, or repetitive contraction and relaxation of the PFM in order to strengthen them. For someone with true pelvic pain Kegels are not the answer, especially in the beginning. Your therapist will first give you stretches that help your PFM fully relax. Once you’ve learned to establish a healthy resting tone, then it is safe to begin strengthening the muscles with Kegels. It is essential that you have a therapist to give you the right exercises at the right time, in order to achieve full resolution of symptoms.
Pelvic pain can be confusing and scary, but there is help. Pelvic health physical therapists are here to be a part of your medical team, and to work alongside your doctors to make sure you live a healthy and happy life.
Center for Disease Control and Prevention. Trends in Asthma Prevalence, Health Care Use, and Mortality in the United States. 2012- Ahangari, A. Prevalence of Chronic Pelvic Pain Among Women: An Updated Review. Pain Physician. 2014
- Ferris et al. National Prevalence of Urogenital Pain and Prostatitis-Like Symptoms in Australian Men Using the NIH Prostatitis Index. BJUI. 2009 Apr 8.
- Howard F MD, Barberei R MD, Faulk S MD. Causes of Chronic Pelvic Pain in Women. 2011.
- Faubion S, Shuster L, Bharucha A. Recognition and Management of Nonrelaxing Pelvic Floor Dysfunction. Mayo Clin. Proc. 2012.
- Chichowski et al. Sexual Abuse History and Pelvic Floor Disorders in Women. South Med Journal. 2013.
- www.pelvicpain.org