Case Study: Penile Pain
This is a subtitle for your new post
This week we’re reviewing a case of a male patient, 54 y.o, with chief complaint of penile pain. This was a somewhat unusual case because of how soon the patient was referred to us. Typically in men with penile pain, physical therapy is their “last ditch effort” after they’ve tried everything and have been in pain for months. With this client, his pain had only been present for two months before he found our clinic.
He presented to the clinic in March of 2023, his history is noted here:
“The pain started this winter. He was given a urine culture that came back negative but was given antibiotics anyway. They helped but when he stopped, pain came back. He was then prescribed a one month antibiotic, but the pain came back. He reports a steady ache at the tip of the penis. He denies textural or sensation changes and he reports no difficulty with erection or orgasm. Intercourse is aggravating afterwards, but not during. Around this time he was also doing less cycling and more weight lifting. He is not maxing out but doing mostly super sets 30 minutes x 3 per week. When he lifts, that doesn't change the pain for better or worse. Pt works in a high stress sales job with frequent air travel, prolonged sitting aggravates the pain. Pt is an avid cyclist and has been for years, riding x 6 days per week 25-35 miles each time. Cycling does increase his pain. His bike is specifically fitted to him and there have been no recent changes to his bike since the pain started. Pt denies pain with urination but has a mild sensation he isn't emptying fully.”
Where did we start?
When it comes to treating penile pain, the trick is to remember this: it’s almost never the penis itself! It is commonly caused by tension in the muscles and nerves that supply feeling and blood flow to the penis. Our first visit involved assessing the following areas for tension, pain, and/or decreased flexibility:
- Abdominal wall
- Hips
- Low back
- Thighs
The patient had limited motion in his lumbar spine (difficulty rotating to the right and the left), and his muscles were especially tight in his hamstrings and inner thigh on the R side. His abdomen was normal, no excessive tension there, although the abdominal wall can be a common culprit for penile pain. I also noticed he had very tight hips and poor range of motion on each side. We hadn’t yet assessed his pelvic floor muscles and had already found plenty to work on!
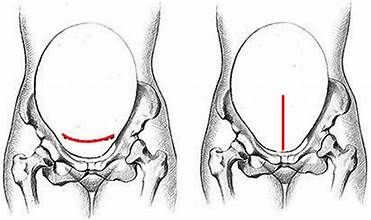
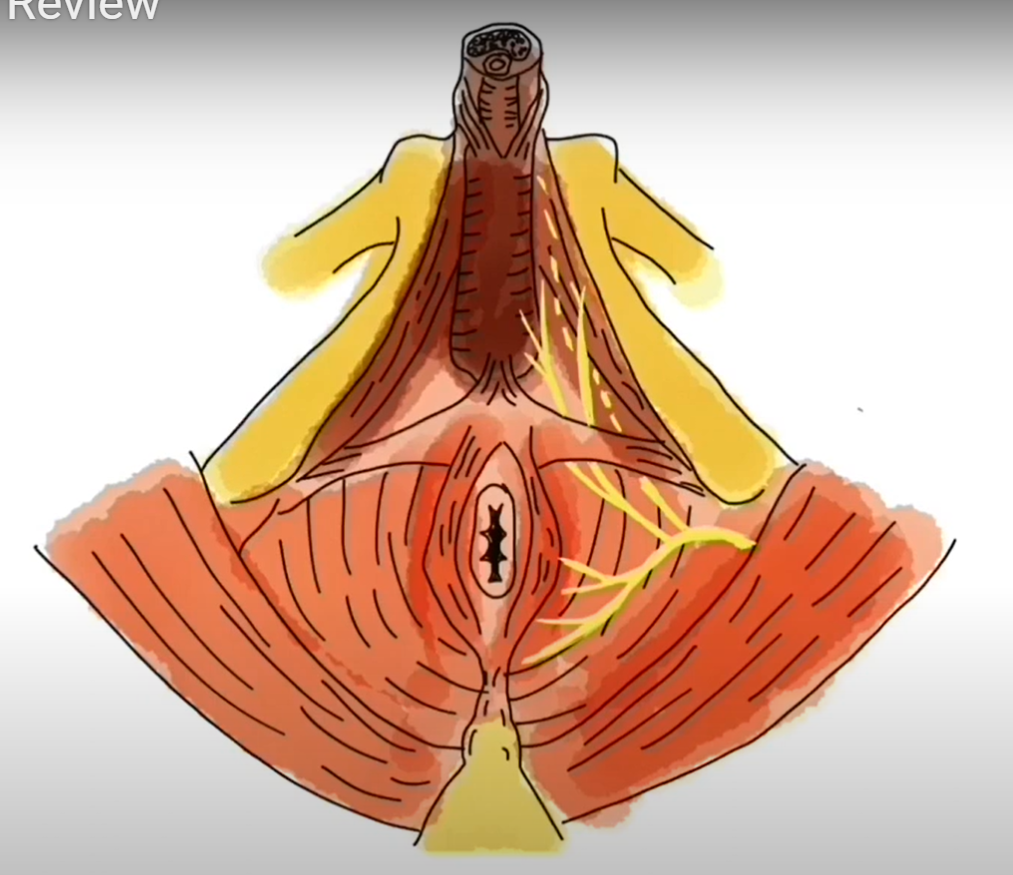
On the next visit, we looked at the pelvis and the nerves and muscles within it. When someone reports penile pain, one of the things we need to rule out is pudendal nerve involvement. This is a small nerve that can wreak havoc on a pelvis if irritated. It directly innervates the areas of the anal opening, perineum (area between rectum and base of penis), and full length of the penis. What you see here is an example of a male lying on his back, and we’re looking at the front of his pelvis: penis along the top, tailbone at the very bottom, and rectum in between. The yellow lines demonstrate the path of the pudendal nerve. If this nerve is irritated, you could have pain anywhere along this distribution.
Here is a detailed video on the anatomy of the male pelvis and the pudendal nerve (Link here)
During the pelvic assessment the patient is disrobed from the waist down, lying on his back on the treatment table, draped with a sheet. From this position I was able to feel all the muscles you see above (pictured in red), and assess for pain. It makes sense that if these muscles are tight, that would create tension around the nerve, leading to irritation and pain. The patient had mild tension here, but nothing we touched reproduced his pain.
The next step is performing an intrarectal exam. Muscles called the levator ani are the muscles we most commonly think of as our “kegel” muscles. These can only be accessed via an intra vaginal or intra rectal exam and if they are tight, can be a direct cause of nerve pain. This patient showed significant muscle tension during his exam, and when I touched the muscle named puborectalis (pictured below), it reproduced his penile pain.
So far, we have significant findings in the following areas:
- Tight hamstrings and middle thigh muscles, with decreased hip joint flexibility
- Significant tension to the muscles inside the pelvis
- Stiff lumbar spine with limited motion
Where did we go from here?
At the next few appointments, we worked on the muscles in his legs and hips to promote relaxation. We also continued with intra rectal pelvic floor muscle release. At the end of each session we would perform hip and lumbar mobility exercises, and the patient was encouraged to continue with these at home.
Two of the main triggers for penile pain were travel and stress. During this time the patient was traveling via car and plane for work, with high stress related to public speaking and work responsibilities on these trips. Each time he would travel and get stressed, his pain would increase. Once he realized the pain was back, he would become more stressed, triggering more pain. We see this often in our pelvic pain patients. We used several strategies to help him through this busy work and travel season:
- He purchased a cushion to sit on when he traveled. He actually purchased a travel neck pillow, but used it as a seat cushion. This significantly reduced his pain with travel, and he didn’t have to feel embarrassed carrying around an extra butt cushion. (Click here for more cushion info)
- We did a LOT of pain science education. The patient felt much more in control once he understood how his pain was working and how he could prevent it.
- The patient was still cycling pretty consistently, but I encouraged him to be mindful of his pain when choosing when, and how long, to cycle. If he was already in pain, we took cycling off the agenda that day.
We’re now into mid April 2023. The patient has had eight visits of PT, once or twice a week for the past month. He’s been on his last work trip of the year and experienced no pain, and continues to cycle with no pain. He was discharged on April 25, 2023 and did not need to return.
II believe he was so successful because he made it to PT quickly after his pain started. If you’re having any type of pelvic pain the sooner we can see, the better!