Case Study: Post Prostate Removal
This is a subtitle for your new post
Today’s case study is one of my favorites, because this patient used physical therapy exactly the way we recommend - and it paid off! This patient is a 62 y.o. male with prostate cancer. He is scheduled for prostate removal January 9, 2023 and presents to PT for prehab in December 2022. Let’s begin with his medical history before his surgery, and then we’ll review his symptoms post surgery.
Pre Surgery History:
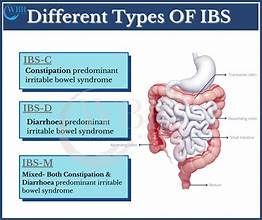
“The patient presents to PT for prehab for RALP (prostate removal) surgery scheduled on Jan 9. He is doing kegels 3 sets of 20 per day currently, mostly quick flicks. He states he can stop the urine stream. He reports history of Ulcerative Colitis but is in remission right now. He exercises by walking about one mile per day”
Where do we start?
The purpose of seeing a PT prior to prostate removal is to get instruction on how to perform pelvic floor muscle exercises. We know that seeing a therapist PRE surgery gives better results in the short term, following surgery.Typically clients do not need more than 1-2 visits pre - op. There are many ways your therapist can help you understand how to perform pelvic floor muscle training:
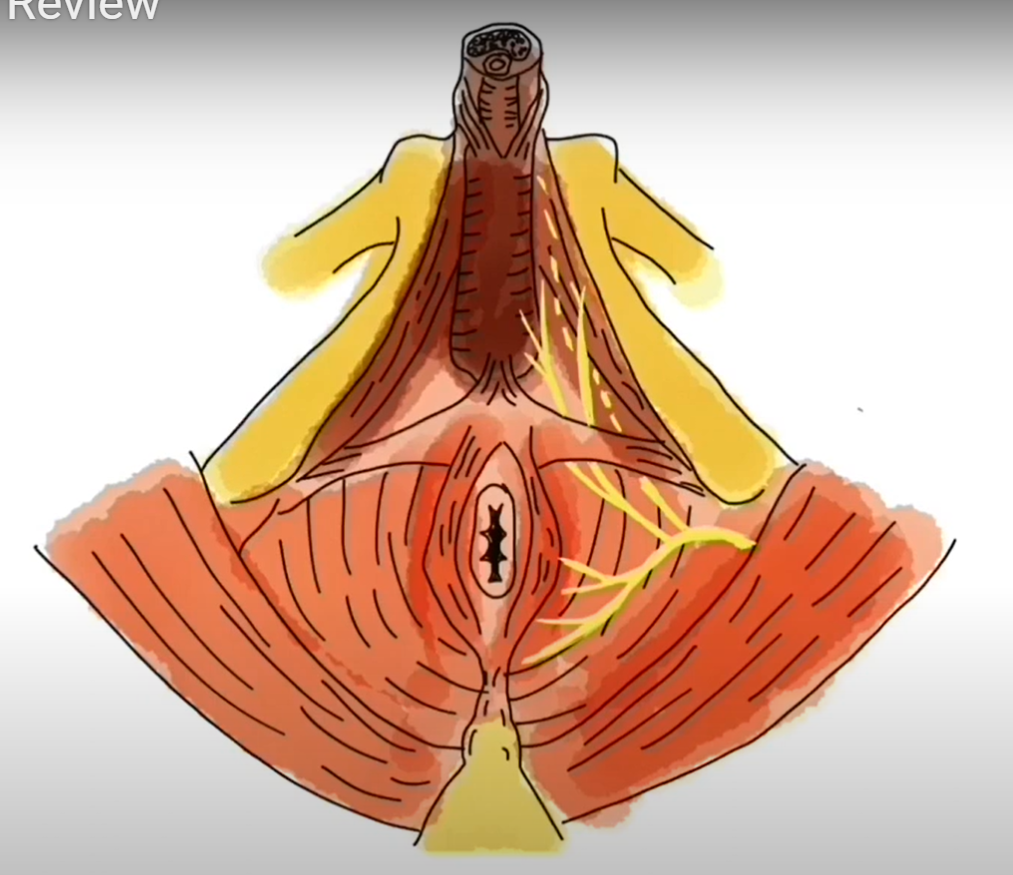
- Biofeedback with external and/or internal sensors (See example here)
- Internal rectal exam
- Verbal instruction for how to contract and relax the pelvic floor
With this particular client, he declined an internal rectal exam and biofeedback. I gave him verbal instruction on how to perform kegels, and gave him a specific routine. I wanted him practicing long endurance holds AND quick contractions daily. Three times per day he would perform 10, 10s contractions and 10 “quick flick” contractions.
I also educated the patient on how to use his breathing diaphragm and his abdominal muscles to reduce the strain on his pelvic floor. Learning to coordinate the pelvic floor, abdomen, and diaphragm is a huge component of post surgery rehab, so we want to train the brain early.
The last portion of a prehab visit includes education on what to expect post surgery. We spoke about the following:
- Having a catheter in, and how long that would be in place (about 10 days)
- When to start kegels again after surgery (once the catheter is removed)
- When to start PT again (once the catheter is out)
- Expectations for erectile dysfunction and potential treatments (Information here)
- The use of penile clamps, how and when to use them (Directions here)
With this client, we were able to cover all of this in one visit, and the next time I saw him was about one month post surgery. Here is his symptom report as of Feb 2023:
“Pt notes leakage while standing, coughing, laughing. He is getting bladder urges but will go more often because it decreases leakage. He had a catheter for 25 days post surgery. He now wears one Depends per day and goes through 6-7 pads within the Depends, per day. He is leaking through the night while asleep. He does 20 kegels at a time, x 3 per day and holds for "a few seconds." He can stop the stream of urine, the urine stream is strong. He reports constipation off and on and is taking Senna daily. Stool is "hard and large." He is taking Cialis and using a penis pump daily.``
Because the patient had a lot of prehab education, he was already managing his constipation and erectile dysfunction well. Had he not been doing these things, I would have recommended oral medication and penile pump for E.D. The symptoms he’s reporting here are extremely common for a man one month post prostate removal.
Where did we start?
We scheduled the patient twice weekly for one month, and then once weekly for another month. At this first session we did an internal rectal exam to test for pelvic floor muscle strength and coordination. The patient was able to contract his muscles well, but had difficulty with complete relaxation. For this reason I recommended biofeedback, which is a tool we use to give patients a visual picture of their muscles working in real time. The patient declined using biofeedback so that was not a part of his treatment plan. I did have him continue with kegel training at the following intervals: 10s contraction x 10 reps, 2s contraction x 10 reps, SIX times per day, all contraction done in standing. (Research here)
A large part of his rehab in the beginning was retraining his abdominal muscles to work together with his pelvic floor. If the patient isn’t able to use these muscles correctly, it ends up creating more pressure on the pelvic floor, resulting in more leakage. The first few visits consisted of table exercises with little to no resistance, making sure the patient was able to coordinate all movements and continue to breath (breath holding is also a common culprit of leakage).
Once the patient was performing the basics better, we transitioned to more functional movements in the gym i.e., sitting, standing, walking, squatting, bending, lifting, etc. With each week, the patient was reporting less and less leakage. His leakage at night was eliminated first, which is the case with most patients. By the end of February the patient had completely eliminated the need for Depends and was using about 5 regular pads per day. His pads at night were dry. Exercises continued to become more challenging in the gym and at home. At the end of March the patient was using 2-3 pads per day, depending on his activity level.
In regards to his erectile function, the patient was still unable to achieve spontaneous erection two months post surgery. This is also extremely common. He was taking oral medication and using the penile pump daily. Although he could not achieve full erections, he was able to achieve orgasms. Because the patient had no trouble with E.D prior to surgery, we expected him to make a full recovery with continued use of meds and the pump.
The patient was discharged after two months of therapy. He was still experiencing leakage but we were confident that his symptoms would continue to improve as long as he was compliant with the kegel program and general strengthening program