Blog
Advanced Physical Therapy

A pessary is a medical device that is inserted into the vagina to provide support for the pelvic organs. It's primarily used in the management of conditions like pelvic organ prolapse (where organs like the bladder, uterus, or rectum drop from their normal position) and urinary incontinence. There are several uses and benefits of pessaries, including: Pelvic Organ Prolapse (POP) : In women with prolapsed organs, the pessary helps to hold the organs in place and prevent them from descending further. It’s often used in cases where surgery isn't an option, or a non-surgical approach is preferred. Urinary Incontinence : Pessaries can help in cases of stress urinary incontinence by supporting the bladder and urethra, thus reducing leakage of urine during activities like coughing or sneezing. Support During Pregnancy : Some women with a weakened pelvic floor or those experiencing symptoms of prolapse during pregnancy may use a pessary to provide additional support. Pessaries come in various shapes and sizes, and they are usually made of medical-grade silicone. A healthcare professional will typically help determine the right type and size for the individual, and the device needs to be cleaned and removed regularly. They are considered a safe and non-invasive option to manage these conditions, but it’s important for users to follow the guidance of their healthcare provider. Patients with symptoms like the ones listed below can often benefit from a pessary: The feeling of, or seeing, something “falling out” of the vagina Heaviness, fullness, pressure inside the vaginal canal Urinary incontinence with coughing, sneezing, laughing, lifting, exercise General heaviness, pressure, dull ache, pulling sensation within the pelvis and lower abdomen Our therapists are trained in pelvic examinations specifically for pessary fittings. The size and shape of the pessary depends on what organ is descended, how significant it is, and your individual vaginal anatomy. If you’re experiencing any of the above symptoms, speak with your gynecologist and ask about the possibility of a pessary. There are special considerations in the post menopausal population for pessary use, most notably vaginal estrogen replacement. With the addition of a medical product inside the vagina, it’s important to make sure the vaginal walls are as healthy as possible. Not every single person is a candidate for vaginal estrogen, but the vast majority of women are. This is a discussion to have with your health care provider prior to pessary fitting. The body content of your post goes here. To edit this text, click on it and delete this default text and start typing your own or paste your own from a different source.
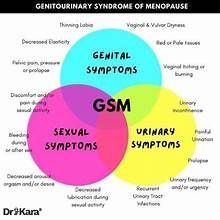
Genitourinary syndrome of menopause (GSM) is a broad term that encompasses all vaginal, sexual, urinary, and pelvic floor symptoms that are associated with a lower-estrogen state (i.e. menopause). These include: Vaginal symptoms Vaginal dryness Burning, pain, irritation, itching, or tears in the tissue of the vulva (external female genitalia) thing/graying of pubic hair Vaginal wall prolapse Vaginal pain or pressure Sexual symptoms Loss of lubrication Pain or bleeding with sex Loss of libido, arousal, or orgasm Urinary symptoms Painful urination Recurrent UTI’s Urinary urgency and frequency Stress , urge, or mixed incontinence Urethral caruncle (red growth on urethra) GSM is more common than you may believe. GSM affects 50% of women by the age of 60 and 75% by the age of 70. Even though this is common many women may feel uncomfortable voicing these symptoms to their medical providers, but the good news is there is treatment! There are several treatments for GSM. Vaginal estrogen is the number one treatment for GSM. Vaginal estrogen is safe with one of the only possible side effects being yeast or thrush although this is not common. Vaginal estrogen can also help prevent bacterial vaginosis (BV) which is an overgrowth of one or more species of normal vaginal bacteria. A lot of women have concerns with estrogen but overall studies have shown vaginal estrogen does NOT increase the risk of cardiovascular disease or cancer. However, it is encouraged to talk to your provider to see if this is an option for you based on your personal medical history. Other treatments for GSM include: Pelvic floor physical therapy can help reduce urinary incontinence, reduce pain, and teach you all of the things to help improve your knowledge of vulvar care. Vaginal moisturizers and lubricants can help with dryness and pain with penetration. Some recommended brands include Good, Clean Love and Replens. There are some products that are better than others (see our previous blog on Lubricants) so be cautious when choosing these products. Diet and lifestyle can make a huge impact beyond just the use of estrogen. Avoiding antibiotics (as much as possible) helps to prevent damage to the microbiome in the vaginal canal. Tobacco use lowers estrogen and also damages the microbiome. Avoid using anything such as wipes or douches that would alter microbiome. The vagina is a self cleaning oven, we do not need anything to clean it! Lastly, exercise and functional activities (our specialty!) for the abdominals and back musculature can help with pelvic floor function. Bottom line: GSM is common, but not talked about enough. Reach out to your provider to voice your concerns regarding your symptoms. There is help!
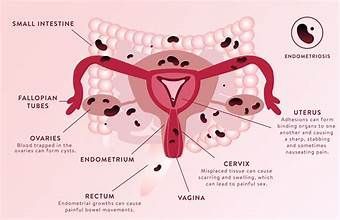
What is Endometriosis? Endometriosis is a disorder in which the tissue that normally lines the inside of your uterus — the endometrium — grows outside your uterus. This endometrium most commonly implants on your ovaries, fallopian tubes and the tissue lining your pelvis. Rarely it can occur beyond the area where pelvic organs are located, like your diaphragm or skeletal muscle. The endometrium acts as uterine tissue and is sensitive to your body's estrogen levels — it thickens, breaks down and bleeds with each menstrual cycle. This is why those folks with endometriosis have a significant increase in symptoms around their period, and also why hormonal birth control that limits periods can be helpful in pain management. The pain from endometriosis is present because this tissue has no way to exit your body, and eventually develops scar tissue and adhesions. What are the symptoms? The most common symptom of endometriosis is pelvic and abdominal pain, but you may also experience any of the following: Painful Periods (sometimes very severe pain) Pain with penetrative sex, pelvic exams, or tampon placement Pain when emptying the bladder or bowels Excessive bleeding during periods and bleeding in between periods Infertility And more…fatigue, diarrhea, constipation, bloating or nausea, especially during menstrual periods What are the risk factors? Several factors place you at greater risk of developing endometriosis, such as: Never having given birth Starting your period at an early age Going through menopause at an older age Short menstrual cycles — for instance, less than 27 days Heavy menstrual periods that last longer than seven days Having higher levels of estrogen in your body or a greater lifetime exposure to estrogen Low body mass index A family history of endometriosis Endometriosis usually develops several years after the onset of menstruation. Signs and symptoms of endometriosis may temporarily improve with pregnancy and may go away completely with menopause, unless you're taking estrogen What treatments are available? Treatment for endometriosis usually involves medication or surgery. The approach you and your doctor choose will depend on how severe your signs and symptoms are and whether you hope to become pregnant. Options for treatment include: Pain management: often in the form of oral medications Hormone therapy: most common type is oral contraceptives Surgeries - excision of the affected tissue, ablations, or hysterectomy PELVIC FLOOR PHYSICAL THERAPY As Pelvic Floor Physical Therapists we cannot “CURE” your endometriosis, but we play a large part in helping you manage the symptoms and get back to a pain free life. In endometriosis, the original “driver” of your pain is the uterine lining that becomes implanted in places other than the uterus. These tissues have their own highway to the brain, and are sending pain signals each time they grow, shed, and bleed. This causes your brain to “sound the alarm” and put the pelvis into a “fight or flight” response. When the brain does this, it does not selectively send an alarm to the uterus alone. It sends the alarm to the entire pelvis: the bowel, bladder, vagina, and pelvic floor muscles. When our pelvic floor muscles receive this alarm, their response is to tighten up, get guarded, and stay that way until they’ve been told there is no more alarm. THIS is where your pelvic health PT/OT comes into play! It’s often very difficult for you as the patient to realize which of your muscles are in this “fight or flight” response. We help you locate the muscle(s), and teach you how to release that tension. People with endometriosis will often also have tension in the muscles of the abdomen, hips, and low back. Pelvic health practitioners are experts in all things bowel, bladder, and sexual dysfunction. We are specialists in working with pelvic and abdominal pain, scar tissue, muscular tightness, and more! Once you’ve received a diagnosis of endometriosis, it’s time to find your pelvic rehab provider. Go to www.pelvicrehab.com to find a practitioner near you!
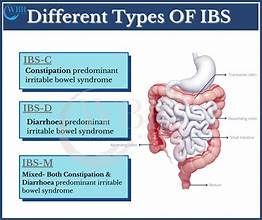
I have heard physicians say that food and nutrition are not important in the management of IBS and other gastrointestinal conditions. As infuriating as that sounds, many other dietitians have shared similar experiences with me. In honor of IBS Awareness Month, let’s learn about this condition and the tremendous effects that food, nutrition, and lifestyle change can have for those with IBS. Approximately 12% of people in the United States have Irritable Bowel Syndrome (IBS), a chronic, functional bowel disorder characterized by symptoms such as bloating, abdominal pain, diarrhea, or constipation. There is no specific test for IBS but at least two of the following must occur once a week for 3 months: pain and discomfort related to defecation, a change in the frequency of defecation, or a change in stool consistency (1). There are three main types of IBS: diarrhea predominant (IBS-D), constipation predominant (IBS-C), and a mixture of the two (IBS-M). Various conditions may need to be ruled out such as Intestinal Bowel Disease (Crohn’s and Ulcerative Colitis) or Celiac Disease. Underlying Causes Etiologies of IBS may be elusive but several that have been proposed by research include foodborne illness, “visceral hyperalgesia [hypersensitivity], intestinal permeability, immune activation, altered gastrointestinal motility, autoimmunity, and alteration of the gut microbiome” (1). Every case is unique, so a general recommendation such as “eat more fiber” could have detrimental repercussions while a suggestion to only “eat what you tolerate” is not very helpful. A comprehensive nutrition and lifestyle assessment is essential. That is why someone with a gastrointestinal disorder should add a registered dietitian to their healthcare team. Conventional Treatments Examples of medications that may be used to control symptoms include antidepressants, prokinetics, antibiotics, pain medications, and laxatives. Their effectiveness varies, and they are often unsuitable for long-term use and carry a risk of side effects. Medications for IBS have often been categorized as “band-aids'' which do not address the root cause of the issue. The relapse rate of symptoms is high, and it is common for someone to spend decades searching for the right treatment and tens of thousands of dollars on tests. You may be asking: “Do you have any good news, then, Nathan?” Yes, I do, but I think it is important to validate the experiences of each and everyone’s health journey and the long road that many with IBS travel to find symptom relief. It breaks my heart to see so many dismissed by their healthcare providers and given lackluster nutrition advice. Flare Ups Before diving into strategies that can address the root causes of IBS, let’s discuss some basic steps to manage symptoms through a food and nutrition lens. After all, it is important to address what to do in a flare up. It is essential to replace fluids and electrolytes lost during periods of frequent diarrhea or vomiting. For constipation, proper hydration is important to help soften stools and encourage their progression through the GI tract. Avoid alcohol, caffeine, and smoking which can irritate the gut and worsen IBS symptoms. Avoid high fat foods (such as fried food, full fat dairy, and processed meat) and spicy foods. Ask your dietitian how much fiber to consume and choose cooked vegetables over raw and softer fruits such as bananas. Eat small, frequent meals and snacks, opting for pureed or liquid consistency (like a meal replacement shake) as needed. Watch out for sugar alcohols (sorbitol, erythritol, mannitol, xylitol, isomalt, maltitol, lactitol) which are one of the most common triggers for gastrointestinal symptoms. They are often used in place of sugar in sugar-free foods and beverages. Eat sitting down in a relaxed setting, chewing food thoroughly, and taking deep breaths. Try to reduce stress as much as possible and consider a free guided meditation video. Avoid strenuous exercise and get plenty of sleep and rest. Low FODMAP Diet The Low Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols (FODMAP) diet is one of the most popular dietary approaches to reduce IBS symptoms, though it is certainly not the only one. Monash University, which created the Low FODMAP diet, explains that FODMAPs are short-chain carbohydrates that may not be absorbed properly in the gut, drawing water into the intestines. They are also highly fermented by gut bacteria, which cause gas. Let me be clear, the FODMAP content alone does not determine if a food is nutrient-dense or not. Some of the healthiest foods (beans, mango, mushrooms, avocado, watermelon, etc.) are high in FODMAPs while some processed food products are high in FODMAPs (like high fructose corn syrup). The goal of the Low FODMAP diet, like any elimination diet, is to reintroduce foods to keep as many foods as possible in someone’s diet moving forward. Some limitations of the low FODMAP diet include that 1) it is restrictive and can be challenging to follow 2) around 30% do not achieve significant symptom relief and 3) it still does not determine the “root cause” of what is triggering symptoms in the first place. SIBO and IMO If you have heard of gut bacteria, probiotics, or the gut microbiome, then you may know that bacteria in the intestines provide many essential health benefits from improved function tobetter digestion to improved cardiovascular health. Many trillions of these bacteria are located in the large intestine while not so many reside in the small intestine. If you have an improper balance of the different types of gut bacteria, it is called gut dysbiosis. If there are too many bacteria in the small intestine, it is a condition called small intestinal bacterial overgrowth (SIBO). Research suggests that as many as half of people with diarrhea-predominant irritable bowel syndrome have SIBO (2). Recently, a new condition (intestinal methanogenic overgrowth) was identified that is related to but different from small intestinal bacterial overgrowth. Intestinal methanogen overgrowth (IMO) is more often associated with constipation while SIBO is often associated with IBS-D or IBS-M. The practical way of testing for SIBO or IMO is a breath test that detects levels of hydrogen, methane, and hydrogen sulfide. Identifying the presence of SIBO or IMO is very helpful for determining treatment options for IBS, but the road to symptom relief can still be quite difficult. There are two antibiotics that can be effective for the treatment of SIBO or IMO: xifaxan and nystatin. Sadly, the relapse rate is very high. Limited research indicates that herbal antimicrobials may work just as well (3). Probiotics can help, and three brands in particular have many supporting studies: VSL#3, LacClean, and Visbiome. However, there should be caution since probiotics can also make symptoms worse. Yet once again, what is the root cause? What caused the bacterial overgrowth in the first place? There are multiple proposed etiologies including motility problems, overuse of proton pump inhibitors, and adhesions caused by abdominal surgeries. Addressing the root cause can help prevent relapse of symptoms. Stress The gut and brain are connected via the vagus nerve, part of the parasympathetic nervous system, which plays a major role in controlling digestion. There is no doubt that stress can greatly affect IBS. For instance, nerves in the gut may be hyper-sensitive, registering more pain from bloating for someone with IBS than for someone without the condition. Stress-reducing approaches, such as yoga, have been studied extensively with good success in reducing IBS symptoms. Conclusion There are a multitude of approaches for treating IBS and each one claims to be “the best.” However, the best approach for alleviating the symptoms of irritable bowel syndrome is to determine the root cause and that varies from person to person. Long-term symptom relief requires a lot of patience, but my hope is that it will not require more blood, sweat, and tears than is absolutely necessary. Medications might bring short-term relief, but their use should be evaluated critically with the knowledge that they could even make symptoms worse over time. Complementary approaches that address food, lifestyle, and stress are essential, and a registered dietitian is a valuable addition to the treatment team.
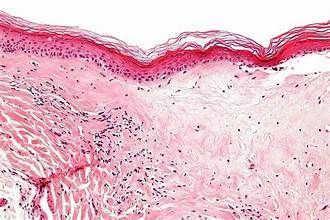
Lichen sclerosus (LS) is an inflammatory, auto immune skin condition that can affect any area of the body. It is most common in the skin around the genitals and causes the tissues to become pale, thin, and tight. Lichen sclerosus can affect both men and women, but more commonly presents in post menopausal women. The hallmark sign of LS is white patches (sometimes shaped like a figure of 8 or a keyhole) around the genital region that can itch, crack, tear, and cause pain with intercourse. In males, it can create narrowing of the opening at the end of the penis, causing difficulty urinating. In females, it can create restriction around the vagina, clitoris, and anus, making intercouse and bowel movements painful. The cause of LS is unknown, but it can be related to hormonal changes, trauma, and immune dysfunction. It is not contagious and is not spread by sexual contact. This condition may be more common than we realize, as we are seeing more and more cases in young females in the clinic. Treatment for lichens generally consists of steroid ointment that reduces inflammation and restores plumpness to the tissues. The goal is to reduce scarring, reduce pain and itching, and improve tissue color and quality. I have seen patients improve DRAMATICALLY after even just two weeks of using the creams as prescribed. Pelvic therapy is imperative in this population. When you have pain in the genital area the pelvic floor muscles can also become tight and tense, leading to more pain. When our muscles become tight, this creates more problems like painful urination, urinary leakage, vaginal tearing, and painful intercourse. Once you've started taking the prescribed medication, the muscles still need rehab! A specialized pelvic floor therapist can perform a vaginal exam, testing for muscle tension and strength. For the vast majority of patients with LS, the goal is to relax and lengthen the pelvic floor muscles - NOT to squeeze, kegel, or strengthen. Your therapist will apply gentle manual therapy to help restore tissue nutrition, increase blood flow, and improve mobility. This reduces the risk of tissue scarring, and also decreases your pain. They will also teach you proper stretches and techniques that you can perform at home. Your pelvic PT/OT will also teach you about the importance of gut health, vaginal pH balance, and reducing acidity in your diet. All of these things together help reduce the severity of LS on your quality of life. So not only can therapy help improve tissue health, but mental health! This condition can be distressing, but medical and therapeutic interventions can restore the quality of your tissues and quality of life! If you have been diagnosed with lichen sclerosus, you can talk to a pelvic health therapist about treatment. This is a treatable problem, and most insurances cover therapy services. We are here to help you on your journey to restoring great health!
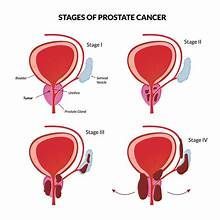
Today’s case study is one of my favorites, because this patient used physical therapy exactly the way we recommend - and it paid off! This patient is a 62 y.o. male with prostate cancer. He is scheduled for prostate removal January 9, 2023 and presents to PT for prehab in December 2022. Let’s begin with his medical history before his surgery, and then we’ll review his symptoms post surgery. Pre Surgery History: “The patient presents to PT for prehab for RALP (prostate removal) surgery scheduled on Jan 9. He is doing kegels 3 sets of 20 per day currently, mostly quick flicks. He states he can stop the urine stream. He reports history of Ulcerative Colitis but is in remission right now. He exercises by walking about one mile per day” Where do we start? The purpose of seeing a PT prior to prostate removal is to get instruction on how to perform pelvic floor muscle exercises. We know that seeing a therapist PRE surgery gives better results in the short term, following surgery.Typically clients do not need more than 1-2 visits pre - op. There are many ways your therapist can help you understand how to perform pelvic floor muscle training: Biofeedback with external and/or internal sensors ( See example here ) Internal rectal exam Verbal instruction for how to contract and relax the pelvic floor With this particular client, he declined an internal rectal exam and biofeedback. I gave him verbal instruction on how to perform kegels, and gave him a specific routine. I wanted him practicing long endurance holds AND quick contractions daily. Three times per day he would perform 10, 10s contractions and 10 “quick flick” contractions. I also educated the patient on how to use his breathing diaphragm and his abdominal muscles to reduce the strain on his pelvic floor. Learning to coordinate the pelvic floor, abdomen, and diaphragm is a huge component of post surgery rehab, so we want to train the brain early. The last portion of a prehab visit includes education on what to expect post surgery. We spoke about the following: Having a catheter in, and how long that would be in place (about 10 days) When to start kegels again after surgery (once the catheter is removed) When to start PT again (once the catheter is out) Expectations for erectile dysfunction and potential treatments ( Information here ) The use of penile clamps, how and when to use them ( Directions here ) With this client, we were able to cover all of this in one visit, and the next time I saw him was about one month post surgery. Here is his symptom report as of Feb 2023: “Pt notes leakage while standing, coughing, laughing. He is getting bladder urges but will go more often because it decreases leakage. He had a catheter for 25 days post surgery. He now wears one Depends per day and goes through 6-7 pads within the Depends, per day. He is leaking through the night while asleep. He does 20 kegels at a time, x 3 per day and holds for "a few seconds." He can stop the stream of urine, the urine stream is strong. He reports constipation off and on and is taking Senna daily. Stool is "hard and large." He is taking Cialis and using a penis pump daily.`` Because the patient had a lot of prehab education, he was already managing his constipation and erectile dysfunction well. Had he not been doing these things, I would have recommended oral medication and penile pump for E.D. The symptoms he’s reporting here are extremely common for a man one month post prostate removal. Where did we start? We scheduled the patient twice weekly for one month, and then once weekly for another month. At this first session we did an internal rectal exam to test for pelvic floor muscle strength and coordination. The patient was able to contract his muscles well, but had difficulty with complete relaxation. For this reason I recommended biofeedback, which is a tool we use to give patients a visual picture of their muscles working in real time. The patient declined using biofeedback so that was not a part of his treatment plan. I did have him continue with kegel training at the following intervals: 10s contraction x 10 reps, 2s contraction x 10 reps, SIX times per day, all contraction done in standing. ( Research here ) A large part of his rehab in the beginning was retraining his abdominal muscles to work together with his pelvic floor. If the patient isn’t able to use these muscles correctly, it ends up creating more pressure on the pelvic floor, resulting in more leakage. The first few visits consisted of table exercises with little to no resistance, making sure the patient was able to coordinate all movements and continue to breath (breath holding is also a common culprit of leakage). Once the patient was performing the basics better, we transitioned to more functional movements in the gym i.e., sitting, standing, walking, squatting, bending, lifting, etc. With each week, the patient was reporting less and less leakage. His leakage at night was eliminated first, which is the case with most patients. By the end of February the patient had completely eliminated the need for Depends and was using about 5 regular pads per day. His pads at night were dry. Exercises continued to become more challenging in the gym and at home. At the end of March the patient was using 2-3 pads per day, depending on his activity level. In regards to his erectile function, the patient was still unable to achieve spontaneous erection two months post surgery. This is also extremely common. He was taking oral medication and using the penile pump daily. Although he could not achieve full erections, he was able to achieve orgasms. Because the patient had no trouble with E.D prior to surgery, we expected him to make a full recovery with continued use of meds and the pump. The patient was discharged after two months of therapy. He was still experiencing leakage but we were confident that his symptoms would continue to improve as long as he was compliant with the kegel program and general strengthening progra m
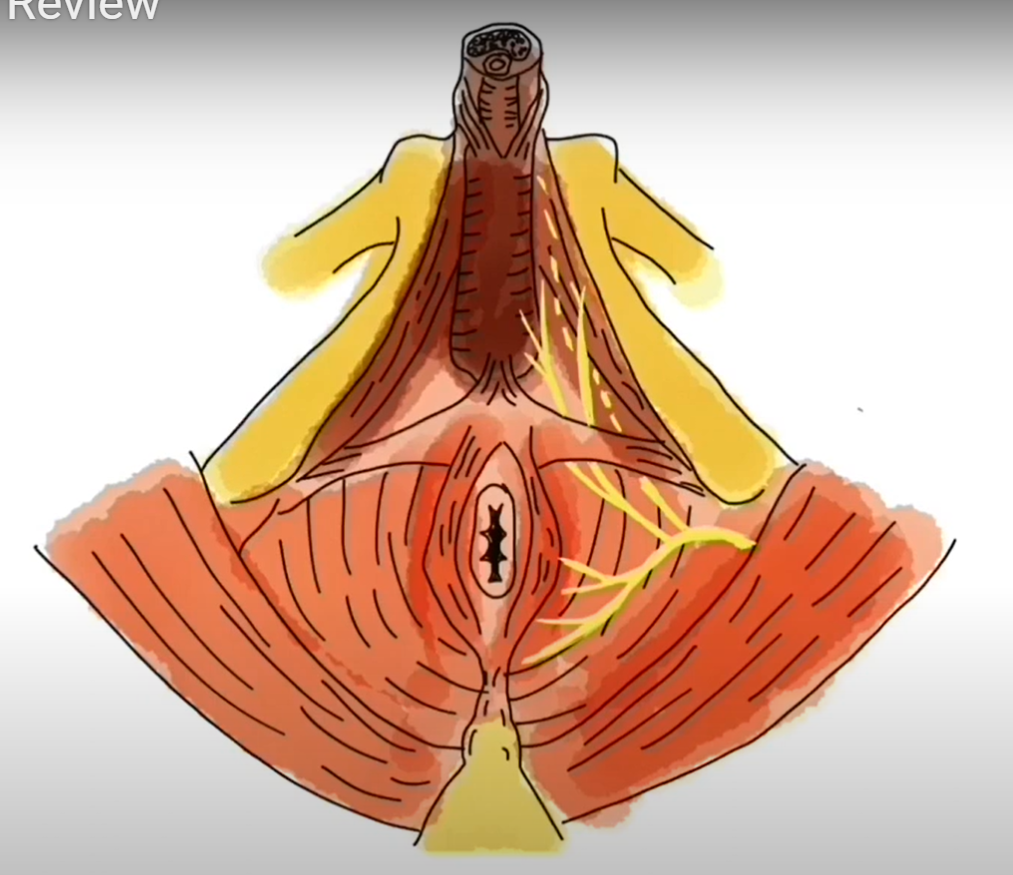
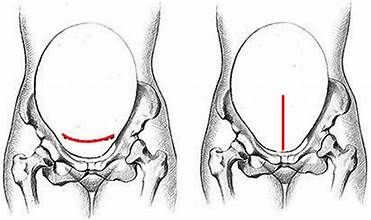
This week we’re reviewing a case of a male patient, 54 y.o, with chief complaint of penile pain. This was a somewhat unusual case because of how soon the patient was referred to us. Typically in men with penile pain, physical therapy is their “last ditch effort” after they’ve tried everything and have been in pain for months. With this client, his pain had only been present for two months before he found our clinic. He presented to the clinic in March of 2023, his history is noted here: “The pain started this winter. He was given a urine culture that came back negative but was given antibiotics anyway. They helped but when he stopped, pain came back. He was then prescribed a one month antibiotic, but the pain came back. He reports a steady ache at the tip of the penis. He denies textural or sensation changes and he reports no difficulty with erection or orgasm. Intercourse is aggravating afterwards, but not during. Around this time he was also doing less cycling and more weight lifting. He is not maxing out but doing mostly super sets 30 minutes x 3 per week. When he lifts, that doesn't change the pain for better or worse. Pt works in a high stress sales job with frequent air travel, prolonged sitting aggravates the pain. Pt is an avid cyclist and has been for years, riding x 6 days per week 25-35 miles each time. Cycling does increase his pain. His bike is specifically fitted to him and there have been no recent changes to his bike since the pain started. Pt denies pain with urination but has a mild sensation he isn't emptying fully.” Where did we start? When it comes to treating penile pain, the trick is to remember this: it’s almost never the penis itself! It is commonly caused by tension in the muscles and nerves that supply feeling and blood flow to the penis. Our first visit involved assessing the following areas for tension, pain, and/or decreased flexibility: Abdominal wall Hips Low back Thighs The patient had limited motion in his lumbar spine (difficulty rotating to the right and the left), and his muscles were especially tight in his hamstrings and inner thigh on the R side. His abdomen was normal, no excessive tension there, although the abdominal wall can be a common culprit for penile pain. I also noticed he had very tight hips and poor range of motion on each side. We hadn’t yet assessed his pelvic floor muscles and had already found plenty to work on! On the next visit, we looked at the pelvis and the nerves and muscles within it. When someone reports penile pain, one of the things we need to rule out is pudendal nerve involvement. This is a small nerve that can wreak havoc on a pelvis if irritated. It directly innervates the areas of the anal opening, perineum (area between rectum and base of penis), and full length of the penis. What you see here is an example of a male lying on his back, and we’re looking at the front of his pelvis: penis along the top, tailbone at the very bottom, and rectum in between. The yellow lines demonstrate the path of the pudendal nerve. If this nerve is irritated, you could have pain anywhere along this distribution. Here is a detailed video on the anatomy of the male pelvis and the pudendal nerve ( Link here ) During the pelvic assessment the patient is disrobed from the waist down, lying on his back on the treatment table, draped with a sheet. From this position I was able to feel all the muscles you see above (pictured in red), and assess for pain. It makes sense that if these muscles are tight, that would create tension around the nerve, leading to irritation and pain. The patient had mild tension here, but nothing we touched reproduced his pain. The next step is performing an intrarectal exam. Muscles called the levator ani are the muscles we most commonly think of as our “kegel” muscles. These can only be accessed via an intra vaginal or intra rectal exam and if they are tight, can be a direct cause of nerve pain. This patient showed significant muscle tension during his exam, and when I touched the muscle named puborectalis (pictured below), it reproduced his penile pain. So far, we have significant findings in the following areas: Tight hamstrings and middle thigh muscles, with decreased hip joint flexibility Significant tension to the muscles inside the pelvis Stiff lumbar spine with limited motion Where did we go from here? At the next few appointments, we worked on the muscles in his legs and hips to promote relaxation. We also continued with intra rectal pelvic floor muscle release. At the end of each session we would perform hip and lumbar mobility exercises, and the patient was encouraged to continue with these at home. Two of the main triggers for penile pain were travel and stress. During this time the patient was traveling via car and plane for work, with high stress related to public speaking and work responsibilities on these trips. Each time he would travel and get stressed, his pain would increase. Once he realized the pain was back, he would become more stressed, triggering more pain. We see this often in our pelvic pain patients. We used several strategies to help him through this busy work and travel season: He purchased a cushion to sit on when he traveled. He actually purchased a travel neck pillow, but used it as a seat cushion. This significantly reduced his pain with travel, and he didn’t have to feel embarrassed carrying around an extra butt cushion. ( Click here for more cushion info ) We did a LOT of pain science education. The patient felt much more in control once he understood how his pain was working and how he could prevent it. The patient was still cycling pretty consistently, but I encouraged him to be mindful of his pain when choosing when, and how long, to cycle. If he was already in pain, we took cycling off the agenda that day. We’re now into mid April 2023. The patient has had eight visits of PT, once or twice a week for the past month. He’s been on his last work trip of the year and experienced no pain, and continues to cycle with no pain. He was discharged on April 25, 2023 and did not need to return. II believe he was so successful because he made it to PT quickly after his pain started. If you’re having any type of pelvic pain the sooner we can see, the better!
Persistent genital arousal disorder, or PGAD, is the unwanted sensation of genital arousal that is not resolved with orgasm. It is classified as a pain disorder, not a sexual disorder, and is characterized by throbbing, tingling, pain, tension, or irritation in the genitals with or without spontaneous orgasm. It occurs without sexual interest and is distracting and, at times, debilitating. The underlying cause of PGAD is uncertain, but it can be related to or associated with certain medications, cysts, anxiety, stress, scar tissue, constipation, bladder dysfunction, pudendal nerve dysfunction, surgery, IBS, or a prolonged period of genital irritation. Treatment for PGAD varies, but may include tri-cyclic antidepressants, transcutaneous electrical nerve stimulation, botox injections, hormone or anesthetic creams, and physical therapy. How can physical/occupational therapy help with something that doesn’t seem… well, related to physical therapy? Pelvic health therapy is extremely beneficial in the treatment of PGAD, because its aim is to calm a sensitized nervous system and the tight muscles that can result. When patients experience PGAD, the nervous system becomes alerted that something is amiss, so the pelvic floor muscles tighten in order to “protect” the area involved. This compounds nerve compression and restricts blood flow to the pelvic structures, leading to trigger points, and an even MORE sensitized nervous system. Pelvic health specialists work with gentle manual techniques to release tight muscles and connective tissue restrictions, as well as instruct patients in how to manage symptoms. This may include leg and pelvic stretches, breathing and postural exercise that maximize neuromuscular function, the use of a device at home to help release tight muscles, or the use of a TENS unit (transcutaneous electrical stimulation) to calm the nerves in the area. Pelvic specialists are also skilled in techniques that address pudendal nerve hypersensitivity and abnormal signaling. Your therapist will address any scar tissue restrictions you may have from endometriosis or abdominal surgeries, as these can contribute to PGAD. Constipation and/or bladder dysfunction will also be discussed and treated. Many patients with PGAD suffer in silence. Please know that there is help available to you! Yes, there is therapy for that! Let us help relieve the symptoms that are keeping you from enjoying life to its fullest.
Our patient presented three days after her Cesarean delivery . This was her third C section, and recovery from her previous two had been no problem at all. Since her delivery she was having sharp, stabbing, 10/10 pain in the left lower portion of her abdomen. She went to see her O.B. who cleared her scar and ensured there was no infection, and sent her to us. (The perfect course of action, might I add. The answer here is NOT to "wait and see if the pain goes away.") The patient admitted she was nervous to go to PT because she could barely walk. She couldn't pick up her new baby girl, could barely go to the bathroom without pain. She was nervous we were going to put her through the ringer in the gym! But luckily she came, and after one visit has cut her pain in half. The first visit consisted of gentle massage and manual therapy to her abdominal muscles. Because she was only three days post delivery at the time of this visit, she had steri strips on her scar. We typically recommend gentle touch around the scar up to 6 weeks PP. Then once the scar is fully healed and cleared, we can begin touch and gentle massage on the scar. Our PT also encouraged the use of a TENS unit ( Linked here ). The nerves that supply the abdomen and groin start in the mid/lower spine, wrap around to the front of the body and continue down towards the vulva/groin. This group of nerves are typically the ones to be irritated post cesarean. We can use a TENS unit for pain relief along the pathway of these nerves. In this particular patient, we used TENS electrodes placed as pictured below in white squares: to the midback at the level of your bottom rib, and directly on the area of pain on the abdomen. The patient was encouraged to use the TENS unit daily, along with ice to her abdomen. You should not use a TENS unit if you have any of the following: Cardiac pacemaker or difibrillator Spinal stimulator for pain or otherwise Numbness or decreased sensation to area where you will place the TENS Diabetic neuropathy The patient did this consistently over the weekend and returned the following Monday with signifciantly less pain. Amazing! Her next session we continued massage along her painful areas, and began doing very gentle deep core activation and deep breathing. This will help her low back feel more supported during the day, and will keep that irritated nerve happy with gentle movement and good blood supply. As her pain continues to decrease, we will do less manual therapies and progress her towards core exercise. The thing we cannot stress enough about this patient is - get here sooner rather than later! Sharp, intense pain is not normal following a Cesarean. If you have any of these symptoms, be sure to call your OB and your physical therapist as soon as it starts. If this patient, or her OB, had let the pain drag on without intervention, it would be a much longer fix.

