Case Study: Young Lawyer with Cystitis
This is a subtitle for your new post
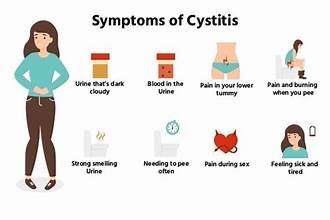
Today’s case study is a 22 year old female, with complaints of life long “cystitis.” We’ll start with her symptom report:
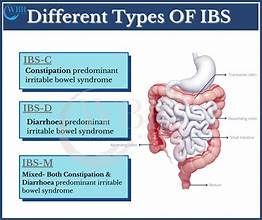
“Pt notes kidney reflux for years as a child, so she assumed all of her symptoms were from that. Since the start of her cystitis her kidneys have been "cleared." She has had PVR testing was "a little high but nothing crazy." While her bladder is filling she feels discomfort especially if she's drinking something other than water. She has painful urination and hesitancy, start and stop urine flow, and her urinary tract will feel irritated for a couple of days. She feels incomplete emptying of her bladder "all the time" but will have these flare ups 3-4 days per week. She notes some form of urinary leakage every day, even when sitting still. She has BMs 1-2x/day, she notes constipation if she's dehydrated or eats lots of carbs. Intercouse is painful but she "pushes through." She feels this has worsened since starting her new birth control (Dospirenone Ethinyl Estradiol)”
Where did we start?
Her first visit was strictly listening to her story, asking questions, and educating on anatomy of the pelvic floor muscles. We spoke about what therapy might look like and explained how we would perform an intra vaginal exam at her next appointment. We scheduled the patient for one visit per week, for eight weeks.
At the next appointment, I performed a full body assessment. We looked at the following things:
- Thoracic and lumbar spine motion
- Muscle tension in the abdomen
- Hip motion and muscle tension
- Pelvic floor muscles via vaginal exam
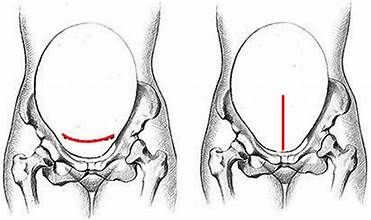
The patient’s spine moved well, and there were no significant findings in her hip joints. Once we got to her abdomen, she was very sensitive. The most tender places were those pictured below:
This makes sense for a number of reasons. She has a long history of bladder irritation and inflammation. Even if her bladder was the reason for her pain, all the muscles surrounding the bladder will become tense and guarded as a result. The patient is also a first year law student, which is a particularly stressful time. One of the most common places we hold our stress is our abdomen (I bet you're gripping your abdomen right now!)
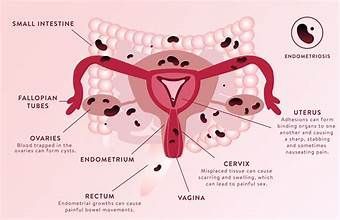
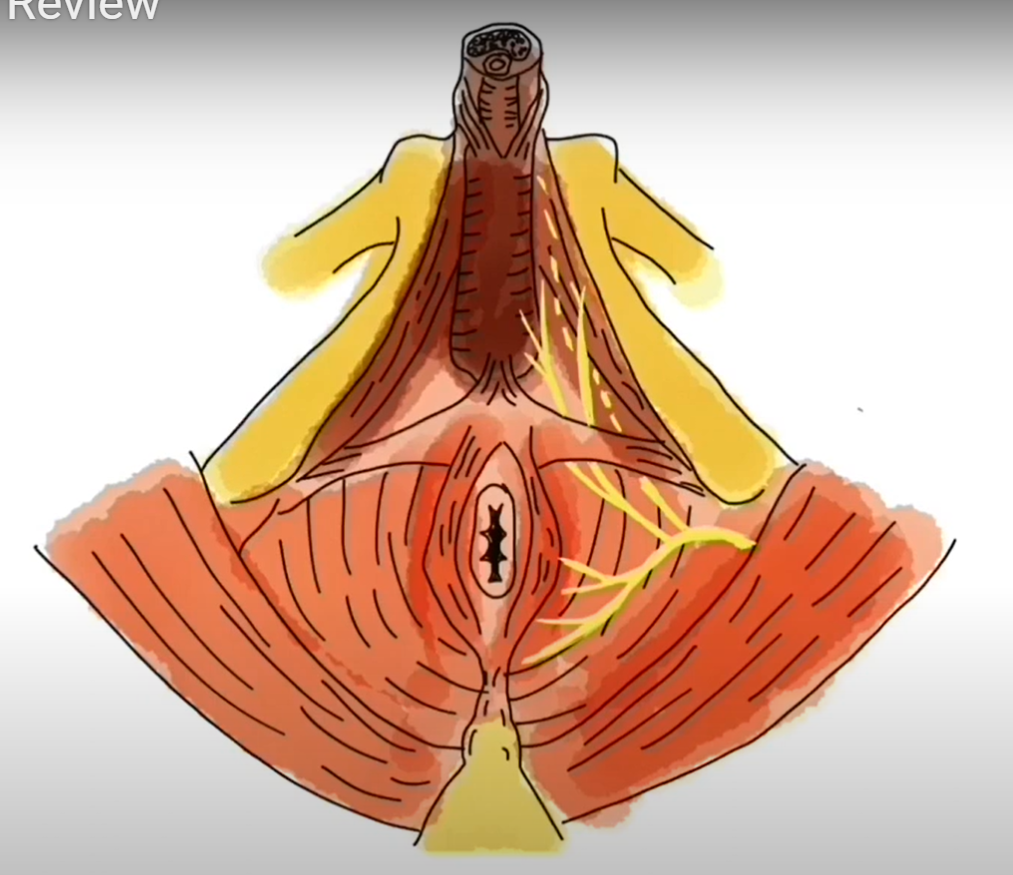
There is also a lot of fascia in and around the bladder. The picture below is a bird's eye view looking down into the pelvis from the top. From top to bottom is the bladder, with the two ureter tubes on either side. The piece in the middle is a cross section of the uterus, and behind that is the rectum.
All of that white, spider webby looking tissue on the right and left of the bladder is fascia. Fascia helps suspend our organs inside the pelvis, and has a tendency to get “stuck” in patients with chronic pain. This was the case for our patient, which is why she had tenderness with touch around the pubic bone/bladder.
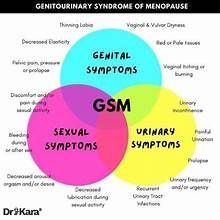
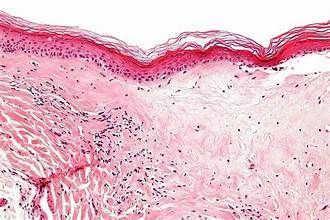
Moving along to her pelvic floor muscle assessment. As a reminder the patient has painful urination, slow urine stream, and pain with sex. When I visualized the skin around her vagina, it was bright red and appeared irritated. She reported burning with touch along the entire right side of the vaginal opening. The patient continued to report burning with an internal vaginal exam. Her muscles inside the pelvis were tight and tense, and performing a kegel made the pain worse. No wonder sex was painful!
After her pelvic exam, I recommended the following:
- Good Clean Love vaginal moisturizer directly to the vulva, vaginal opening and urethra (bladder opening) every night. (Example here)
- An over the counter bladder supplement called D-mannose (Info on D Mannose here)
- Body scanning multiple times throughout the day, specifically checking the tension she’s holding in her abdomen. Being in law school, she needed good tools to check her stress. (How - To Body Scan Here)
- Speak with her gynecologist about other birth control options. Because we know certain birth control pills can increase pain at the vagina, AND the patient stated her pain with sex got worse after starting it, I recommended she ask her GYN for other options.
Her treatment sessions included manual therapy to the muscle groups that were tight and tense, mainly her abdomen and pelvic floor. Trigger point dry needling was used to the muscles in her abdomen, the patient responded very well. At each session we worked on the pelvic floor muscles intra vaginally, applying gentle pressure to tender points until the muscles relaxed. After seven visits, one per week, the patient reported the following:
“Has gotten easier to initiate a stream of urine, and the pain with urination is gone. As her bladder fills throughout the day she denies any pain associated with it. Her constant sense of urgency is much better. In general she states her cystitis is so much better. She still notes leakage 2-3x/day with working out or with standing up, she also notes a small amount after she stands up from the toilet.”
After this visit the patient performed her home program independently for two weeks. At her return visit she reported the only remaining symptom was occasional leakage with heavy lifting during her work outs. That session we reviewed lifting and breathing mechanics, and agreed to follow up in one month. The patient started therapy in October 2022, and was discharged from care symptom free on January 12, 2023.