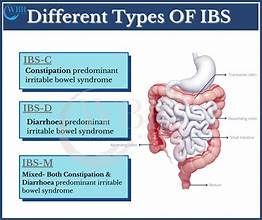
Case Study: 77 Year Old Chronic Constipation
This is a subtitle for your new post
Today we’re sharing the story of a 77 y.o. woman with laxative dependent constipation. We’ll begin with her medical history:
“The patient has been constipated her whole life, she was given enemas as a baby and used laxatives as a teen. Her constipation worsened in 2018 following a hysterectomy and bladder sling surgery. At this point in time, the patient requires prescription medication in order to have a bowel movement. She has tried Linzess but if she takes Linzess alone, the stool will "get down there but I can't get it out." She has recently tried Linzess, Miralax and Docusate and this has been working fairly well. Her GI provider just prescribed Trulance, she will start this week. Her colonoscopies show "redundant colon" but nothing else.”
Where do we start?
Chronic constipation, especially when it is laxative dependent, can take a long time to notice results. Historically the gut is slow to respond to intervention. For this reason I recommended the patient schedule two appointments per week, for ten weeks. As her symptoms improved, we decreased her visit frequency to once per week. She was seen for a total of twelve visits.
In someone with severe constipation, we have to start with the basics. Is the patient getting enough fiber and water in her diet? Is she eating three meals per day? Is she exercising? The answer to all of these questions, for this patient, was yes. This patient was getting on average 30g + of fiber per day, the recommended dose is 25-35g. Her water intake was good (80 + oz per day), she was eating enough calories, and walked regularly for exercise (15-30 minutes per day).
Once I knew she had the basics down, we started her on a home bowel program. Her intestines were not moving on their own, they needed the help of a medication. For this reason, her home program would be full of things that encouraged her bowels to process food on their own. We started this patient on a daily bowel routine that included the following:
- Daily bowel massage ( Instructions here )
- TENS unit protocol ( Protocol here ) + ( Amazon TENS Unit )
- When performing bowel massage and TENS, use the senses to our advantage: perform in the same place, at the same time, with the same environment (think lighting the same candle, listening to the same music, watching the same tv show, etc).
- Walking, or some kind of exercise, for 150 minutes per week
- Continue taking prescription medication as prescribed
The patient was taking Trulance, a constipation prescription medication, daily when we started. She was also taking Miralax twice daily. These medications can be very expensive, and one of her main goals was to reduce her need for them. The patient was extremely compliant with her home bowel program, and after the first week of PT I encouraged her to reduce her Miralax to once per day. She was able to do this successfully over the next week, without a regression in symptoms. Over the next few weeks she continued reducing Miralax to ½ dose daily, which is where she remained for the remainder of treatment.
What does treatment look like?
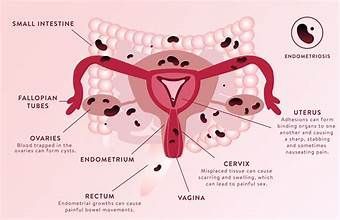
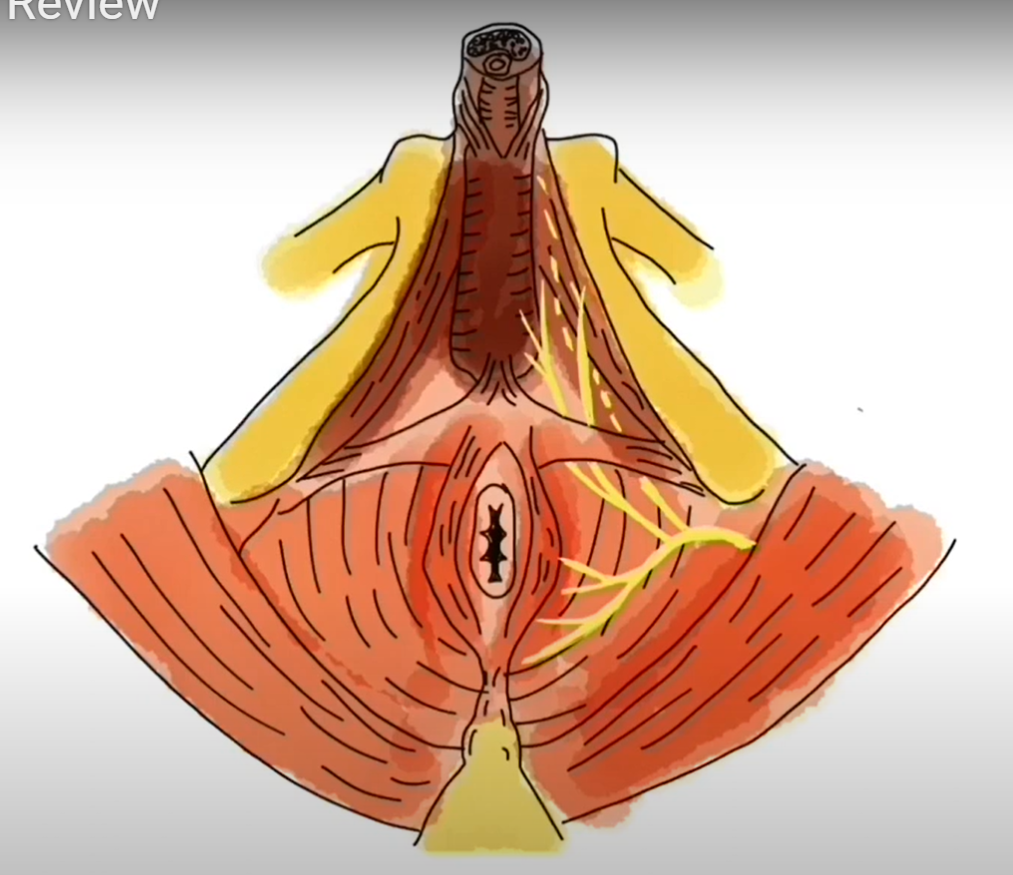
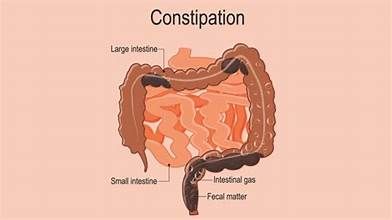
During her sessions, I focused on manual therapy techniques to her abdominal wall. This included bowel massage, along with mobilization to her scars. The patient had a history of multiple abdominal surgeries, and scar tissue can be a factor in constipation. I also mobilized her cecum and sigmoid colon, and the various sphincters within her intestines. ( See anatomy here ). Following treatment to her abdomen, she would perform exercises in the gym focused on abdominal muscle activation and rotation. The deep abdominal muscles lie directly on top of and below the intestines, and contraction of these muscles can promote bowel motility.
As treatment continued, the patient felt comfortable trying days without her Trulance medication. At this point she was having a small bowel movement every day, but only felt fully emptied once or twice per week. I instructed her to skip Trulance on the day following a good, complete BM. It’s very important not to stop these medications “cold turkey,” as your bowels have become used to them. For the first two weeks of weaning, the patient skipped Trulance one day per week. She continued to wean, slowly, until she was taking Trulance twice per week.
Her bowel routine never changed throughout this entire process, she was still doing daily bowel massage and using her TENS unit. By the end of her twelfth visit, she was having some form of a bowel movement almost every day, and was thrilled.
There are many other things we could have addressed. Most people with constipation have tension in their pelvic floor muscles around the anus, preventing them from emptying all the way. The patient we reviewed here did not have that issue, so we did not spend time working directly with her pelvic floor muscles.
Key Takeaways
- The bowel takes TIME and CONSISTENCY to respond to treatment
- Working with your therapist to find a home bowel program you will actually stick to is key
- This client was already doing very well with diet, but most patients need lots of education on water, diet, fiber, and exercise. Management of our bowels as we age takes effort on many fronts - and these are changes we need to plan to make for a lifetime.