The History of Pelvic Health Therapy
This is a subtitle for your new post

It's Not A Pelvic Revolution, It's a Renaissance
What's a Kegel? Most people think that it is squeezing the muscles of their pelvic floor, which surround the urethra, vagina, and anal openings for exercise. Most people believe that these exercises are relatively new, and have been around only since 1948 when Dr. Arnold Kegel coined the term “Kegel exercise.” Those people would be wrong! The idea of exercising the muscles of the pelvis have been present in recorded history for at least the last 6,000 years. The ancient peoples of China, India, Greece, and Rome all knew how essential a strong pelvic floor was to health and wellness.³ In fact, it was viewed as so important to the ancient Greeks that courtesans would use their muscles to split clay phalluses as a demonstration of their pelvic floor muscle strength.⁴ Surprised? So was I. You see, we aren’t experiencing a pelvic health revolution, we are experiencing a pelvic health renaissance.
Sometime in the interim we landed in the pelvic dark ages when talking about the pelvis and the bodily functions that take place there became taboo. People were treated like they didn’t have pelvises. Women didn’t pee or poop, and they certainly didn’t leak! To see a glimmer of the light we have to fast forward to 1936 when Margaret Morris, a UK physical therapist began describing and teaching pelvic exercise to prevent and treat urinary incontinence, a full twelve years before Dr. Kegel arrived on the scene to claim all the glory.³
Today you most often hear of Kegels being prescribed after pregnancy to deal with “leaking” that is a “normal” part of motherhood. The instructions may range from a description from a doctor or nurse saying, “squeeze like you are trying to stop from urinating,” to a pamphlet explaining how to perform them with written instructions. But, Kegels aren’t just for when we’ve sprung a leak, they do so, so much more. And, here is the kicker, they only work,
as long as they are performed correctly and at the correct time.
Therein lies the problem:
50% of symptomatic women do not perform Kegels correctly when given verbal cues alone.³
What if I told you that 25-35% of people in the United States suffer from urinary incontinence?¹ Or that 50% of pregnant women will suffer from some kind of low back pain during their pregnancy?² What if these two problems were really the same problem? A problem with the control and strength of the deepest muscles in our body. As we continue to come out of the pelvic dark ages, these topics can still feel like “pelvic taboo” and aren’t discussed with the openness and honesty they deserve. The result? People across the country of all ages and genders living with debilitating symptoms in secret. If you’re reading this and thinking “I thought I was the only one!,” you aren’t alone. The good news? There is help! Help that is virtually risk free, beneficial for your overall health, and can put you on the path for complete resolution of your symptoms.
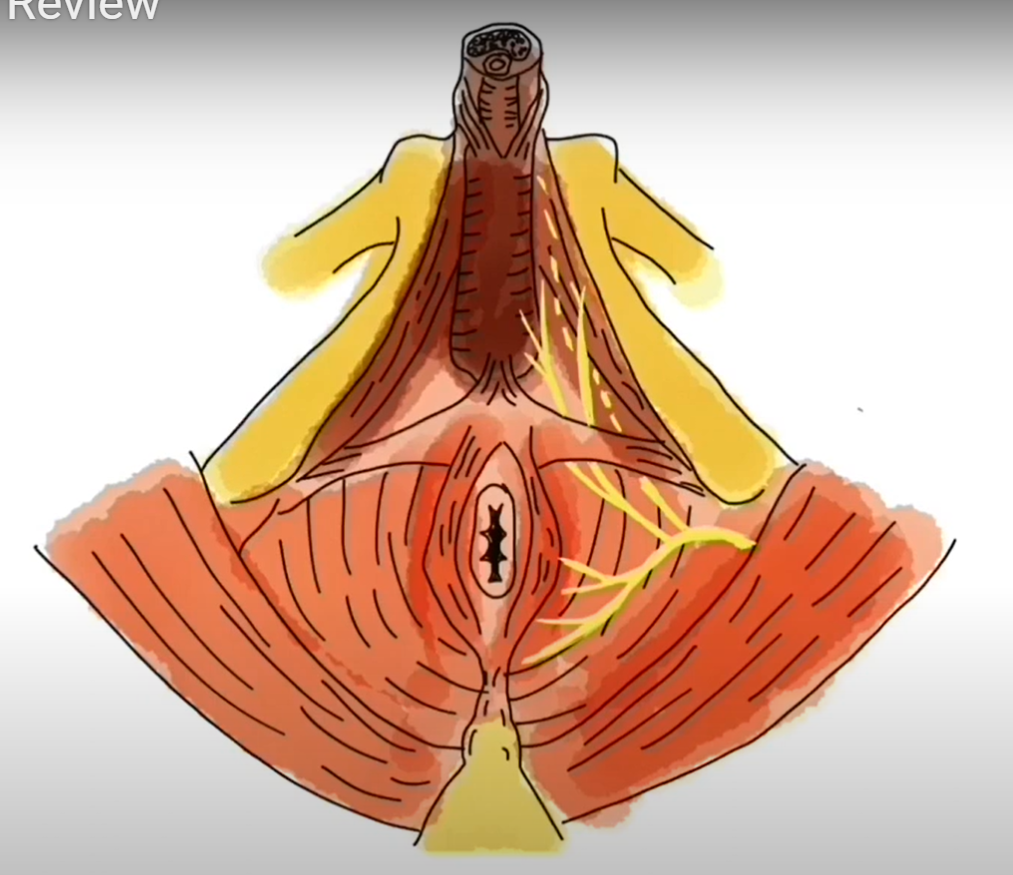
This is where a specialized pelvic health physical therapist can make all of the difference. We specialize in the small group of muscles at the base of the pelvis, often referred to as the “pelvic floor muscles” or the “pelvic diaphragm.” When you perform a Kegel, you are contracting these muscles. A pelvic health physical therapist can help you perform a pelvic floor muscle contraction correctly, and teach you how to translate this new skill to all of your daily activities: walking, standing, lifting, and exercise. On the flip side of the coin, Kegel contractions are not the answer for everybody. If you are having pain with intercourse or gynecological exams, constipation, abdominal pain, or even urinary leakage, performing Kegels routinely may be detrimental. This is another reason why seeing a pelvic health physical therapist can be so beneficial - he or she will be able to prescribe an exercise routine that fits your specific needs.
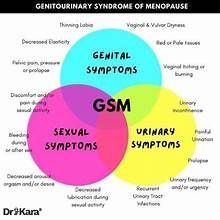
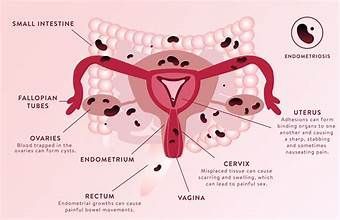
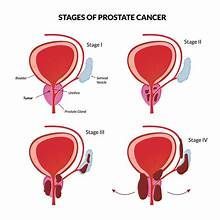
Pelvic floor physical therapy can be beneficial for men and women for a host of diagnoses, some of the most common being:
Urinary and fecal incontinence- Do you ever leak urine, gas, or stool when you cough or laugh? What about when you’re headed to the bathroom and you just can’t quite get there soon enough? Leakage is very common but never normal, regardless of the amount.
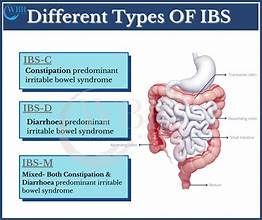
- Constipation
- Are your bowel movements few and far between? Is your stool too hard, making it difficult to pass? Have you gone a week or more without having a bowel movement? There are many factors that contribute to constipation, and your pelvic floor muscles are major players.
- Pain with intercourse
- Is any part of your sexual experience painful? This is a very common report in women and men throughout the lifespan but again, it is not normal. If you’re having pain with tampon insertion, intercourse, gynecological or prostate exams, or sexual climax, it could be due to your pelvic floor muscles.
- Cesarean and episiotomy scar tissue
- Delivery of a baby, no matter how it is delivered, can take its’ toll on the mother. If you had a C-section, you will have scar tissue around the area of the incision. If this tissue is not moved and worked on after your delivery, it can become stiff and painful. The same is true if your doctor had to perform an episiotomy, or a small incision around the vaginal canal, to help deliver your baby. This tissue can also become painful making it difficult to empty your bowel and bladder, have sex, or sit for a long time. This tissue can also be worked on to promote healing and decrease pain.
- Pelvic Organ Prolapse
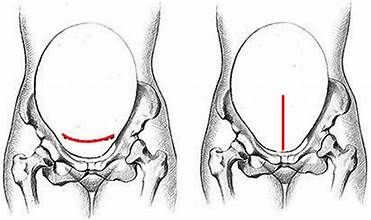
- Have you ever had the feeling that something in the pelvis just doesn’t feel right? That something is hanging a little lower than it should? Sometimes women will report a feeling that their bladder is falling out of their pelvis! This is called pelvic organ prolapse, and is extremely common. Risk factors include increased BMI, 2 or greater pregnancies/deliveries, and chronic constipation. Your pelvic floor muscles contribute to the support of your organs and strengthening these muscles can help in cases of prolapse.
If you are experiencing any of these symptoms you are not alone, and help is available! Stay tuned to upcoming blog posts for details about how pelvic floor physical therapy can help you. Join the Pelvic Renaissance and benefit from the knowledge that has been around for millenia; the muscles at the base of our pelvis are important and we have the power to change them.
Nittis, Victor W. The Prevalence of Urinary Incontinence. Rev Urol. 2001; 3(Suppl 1): S2–S6.
Katonis et al. Pregnancy Related Low Back Pain. Hippokratia. 2011 Jul-Sep; 15(3): 205–210.
Price, Natalia, Rehana Dawood, and Simon R. Jackson. "Pelvic floor exercise for urinary incontinence: a systematic literature review." Maturitas 67.4 (2010): 309-315.
Blackledge C. 48. The story of V: A Natural History of Female Sexuality. Piscataway, NJ: Rutgers University Press; 2004.
Bump et al. Assessment of Kegel Pelvic Muscle Exercise Performance After Brief Verbal Instruction Am J Obstet Gynecol. 1991 Aug;165(2):322-7; discussion 327-9.
Common….Not Normal. Claire Baker. www.youtube.com