FAQ about Pelvic Health Therapy
This is a subtitle for your new post

We’ve all had that one doctor’s appointment that we’d do just about anything to avoid. Maybe it’s a dermatologist appointment to get that mole checked out, or the yearly mammogram, or even your annual check up with your primary care physician. What is it about these appointments that give us that anxious, nervous, “pit in my stomach” feeling? For most of us, I believe it’s the feeling of the unknown, the unanswered questions, the “what ifs” that can really deter us from getting the medical care we need.
This is especially true in the world of pelvic health physical therapy. Imagine this: You’ve been having occasional urinary leakage when your husband makes you laugh really hard. It’s not too bothersome, but you mention it to your OBGYN and he or she refers you to physical therapy. You think, “Physical therapy? I thought that was only for low back pain and total knee replacements?” But you trust your doctor so you make the appointment anyway. As your consultation looms, you begin to think of all the reasons you DON’T want to do this:
- I don’t even talk about this with my partner! Now I have to go talk about my bowel and bladder with a total stranger?
- My friend from college did this once and said they did an internal pelvic exam. What?!
- I mentioned this problem to other medical providers and was dismissed. What is the point of putting myself through that again?
- My main complaint is pain. What if they want to do an examination that will make my pain worse?
- My doctor said they might use some kind of vaginal electrode for treatment. That freaks me out a little bit!
And the list goes on, all of which are completely understandable. This post is here to answer the most frequently asked questions about pelvic health PT, in hopes to ease your mind and give you the confidence to seek treatment.
FAQs About Pelvic Health Physical Therapy
- What will happen at my first appointment?
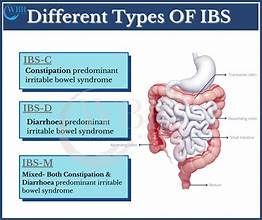
- Your first visit with a pelvic health PT will typically consist of paperwork that gives us an idea of your main complaints (urinary leakage, pain with intercourse, constipation, etc). Once you complete these, you will have a 1 on 1 consultation with your PT. This will involve us asking questions about your bowel, bladder, and sexual health. Your PT will also give education on pelvic anatomy and the pelvic floor muscles, so that you have a better understanding of your specific condition and how PT can help. In most cases, no examination is performed on the first visit. We like to meet you, build rapport, and make sure all of your questions are answered prior to any exam.
- Tell me about this pelvic exam.
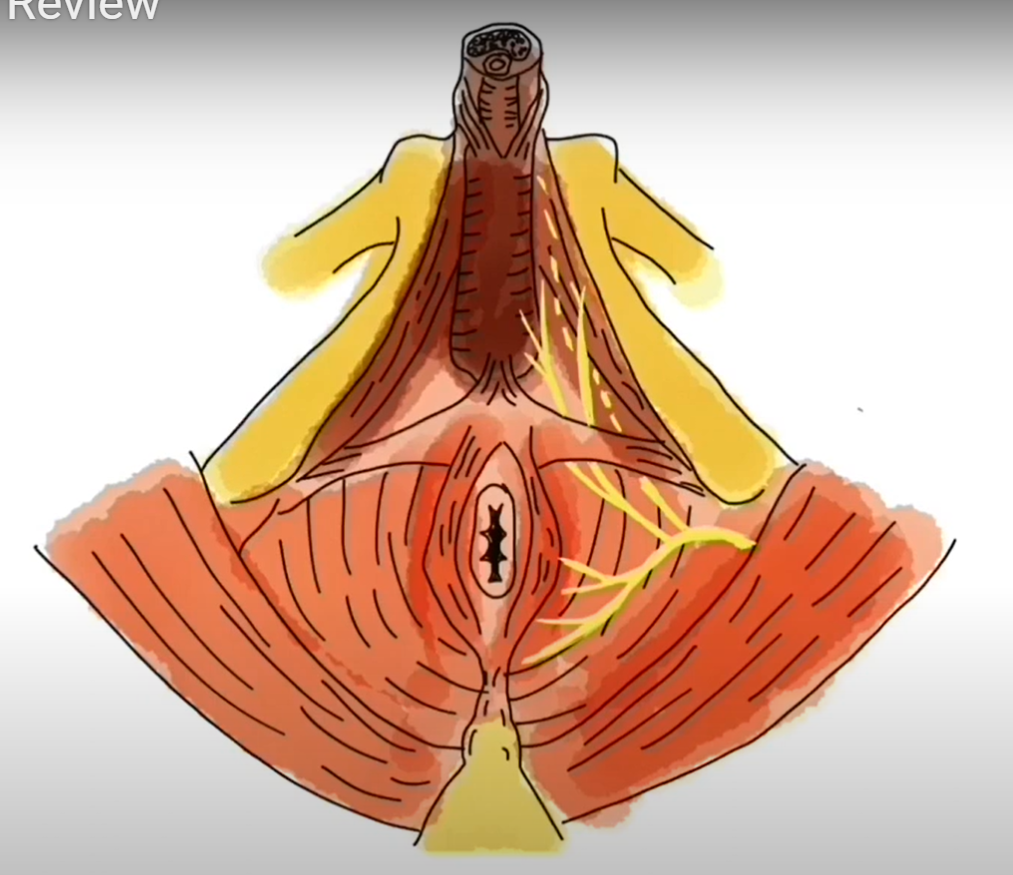
- As physical therapists we are experts in the musculoskeletal system, meaning we treat the muscles and bones of your body. In pelvic health practice, we are able to assess the muscles of your pelvic floor, which are located at the bottom of your pelvis. Because these muscles are located on the inside of our bodies, the best way to assess them is an internal pelvic exam. We do not use a speculum or stirrups during our exams, and we only perform the exam with your complete consent and understanding of all the steps included. Most clients, if not all, will benefit from this exam as it tells us exactly what is going on with your muscles. However, we see plenty of men and women who are experiencing pelvic pain. Would we still perform an exam if it’s painful? In short, it depends.
- If I am in pain, will you still do an exam?
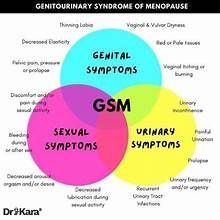
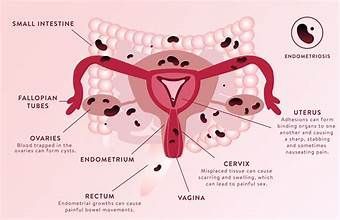
- We see a lot of men and women with pelvic pain, pain with intercourse, abdominal pain, and many other diagnoses that are rooted in pain. When someone is having pain in these areas, the pelvic floor muscles are often over-active, or too tight. Think about it this way: when we get stressed we tend to carry tension in the muscles of our neck and shoulders. After a while, it becomes difficult for these muscles to fully relax and they can become sore, even forming “trigger points” within the muscle. Our pelvic floor muscles can carry tension in the same way, and it can become difficult for them to fully relax as they should. These muscles can become tense for many reasons: stress, pregnancy and delivery, or pelvic organ prolapse to name just a few. Our goal is to teach you to become aware of these muscles and how to relax them voluntarily.
- Everyone’s pain is different, and everyone’s tolerance to a pelvic floor muscle assessment is different. An internal pelvic exam can give us valuable information on the origins of your pain. However, it is very important that your brain begins to have positive, pain free experiences related to your pelvis and your pelvic floor muscles. So if you come to your appointment for an examination and that exam is too painful for you, it is in your best interest that it not be performed until you and your muscles are ready. Your therapist may perform an external examination of the muscles, assess the muscles of your hips, legs, and abdomen, or teach you meditative relaxation techniques. There are a number of things we can do to help you relax these muscles outside of an internal exam, and we can always save the exam for later once your pain has decreased.
- Will I always see the same physical therapist for each visit?
- Due to the sensitive nature of topics discussed during your initial consultation and overall treatment of the PFM, you will always work with the same therapist every single visit. It is so important to build a trusting and positive relationship with your therapist so that you’re able to share details of your signs and symptoms as you progress. This type of relationship can only be reached if you attend each treatment session with the same therapist. This also alleviates the anxiety that can come with sharing your symptoms with multiple people.
- Do you treat men and women?
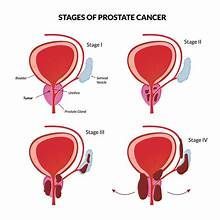
- Yes! Men and women alike have pelvic floor muscles, even though their anatomy is slightly different. It is traditionally thought that women are the only ones who struggle with dysfunction of the pelvis, but men can also experience urinary leakage, pain with intercourse, pain with sitting, and constipation. We can still treat these conditions in men, we just access their PFM with a rectal examination instead of the vaginal examination performed for women.
- What is the vaginal electrode that is sometimes used during therapy?
- Your therapist may use something called biofeedback as a way to re-train your pelvic floor muscles. This involves placing sensors on your muscles and connecting them to a computer. When you squeeze and relax your muscles the sensors show that activity in a graph on the computer screen, so that you are able to see what your muscles are doing in real time. This is a great way for your brain to connect with your muscles, especially since they are on the inside of our body and it’s sometimes hard to tell if we’re activating them in the right way. For biofeedback we can use sensors placed on the outside, or a sensor placed internally into the vaginal or rectal canal. Your therapist will choose which sensor type and placement is most appropriate for you. It’s important to note here that these sensors do not give off any type of sensation to your muscles, and once it is placed you will hardly even notice it’s there.
These are questions we get on a daily basis, but there are many many more to address. Be confident in yourself, and take charge of your own health by asking questions to your medical providers about different options for your pelvic symptoms!