Constipation
This is a subtitle for your new post
We’ve all been there! Maybe it was on that trip to the beach where you got out of your routine, or on vacation when you had to share a bathroom with multiple people. Maybe you just had surgery and are taking pain medication, or you’re eight months pregnant. What do all of these scenarios have in common? They all have the potential for constipation. The dreaded feeling of being bloated and full, feeling like you might never have a bowel movement again. Most of us experience constipation occasionally, three or four times a year. However, there are people who have struggled with this issue for years, since they were children. What causes it? Why do some people deal with it more often than others? What is considered normal and abnormal when it comes to gut and bowel health?
Let’s begin with some common causes of constipation:
- Lack of fiber and water in diet
- The recommended amount of fiber for an adult is 25 - 35 grams per day. Most adults in the U.S. include about half of that in their diet, 15 grams.¹ One way to keep track of your water is to consume half of your body weight in ounces of water per day. For instance, if you weigh 150 lbs, try to drink 75 ounces of water a day.
- Lack of movement or exercise
- Exercise is a natural way to stimulate your gut and get things moving through the intestines. The American Heart Association recommends a starting goal of 150 minutes of exercise per week but if you aren’t able to do that right now, start slow and add in more exercise as your body allows. Talk with your physician before starting an exercise routine.
- Repeatedly delaying or ignoring the urge to have a bowel movement
- Because we can trust our gut to get food and fluids through the system, whenever we get the urge to empty, we should listen. Ignoring the urge to empty your bowels or putting it off for another time can lead to you feeling the urge less often, resulting in constipation.
- Medications
- Various medications, the most common ones being opioids, can cause constipation. Talk with your doctor and read labels for all medications for complete knowledge of side effects.
- Travel, new home, big move, or change in schedule
- Any time we increase the stress in our lives or change up our typical routine, our bowels can suffer. Your gut is a creature of habit - it likes to work in the same environment, with the same scents, and at the same time. Whatever your bowel habits are, it’s best to stick to those as best you can.
How do you know if you’re constipated? With bowel health, it all depends on your definition of “regular.” If you are someone who only empties your bowels once every other day, and each time you do so it is pain free and your stool is of good consistency, that is normal. Consider the “3 and 3” rule when determining what’s normal: 3 bowel movements per day to 3 bowel movements per week. Anywhere in between is considered normal.³
There are a few criteria that help your doctors come to a diagnosis of chronic constipation.They’re listed below, and two or more must be met to be diagnosed with chronic constipation:⁴
- Less than three bowel movements per week
- Manual maneuvers necessary to facilitate defecation more than 25% of the time.
- Hard or lumpy stools more than 25% of the time
- Sensation of incomplete evacuation more than 25% of the time
- Sensation of anorectal obstruction more than 25%of the time
- Straining with defecation more than 25% of the time.
If you have been experiencing two or more of these symptoms for the last 3-6 months, it would be beneficial to see your primary care physician or a gastroenterologist to talk about treatment options. Already seeing a medical provider for your constipation? Ask them about adding a Pelvic Floor PT to your medical management team! It may seem strange to ask a physical therapist for help with your bowels, but depending on the reason for your constipation a PT can be a huge help! Sometimes constipation is caused by dysfunction in your pelvic floor muscles, and more specifically the muscles that surround the anal opening. Having regular bowel movements requires multiple things to go correctly: you need the right amount of water and fiber in your diet, your bowels have to be functioning properly so that they can move things along in a timely manner, and once the stool reaches the rectum to be emptied, your pelvic floor muscles have to be able to relax and allow the stool to pass through.
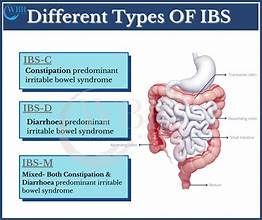
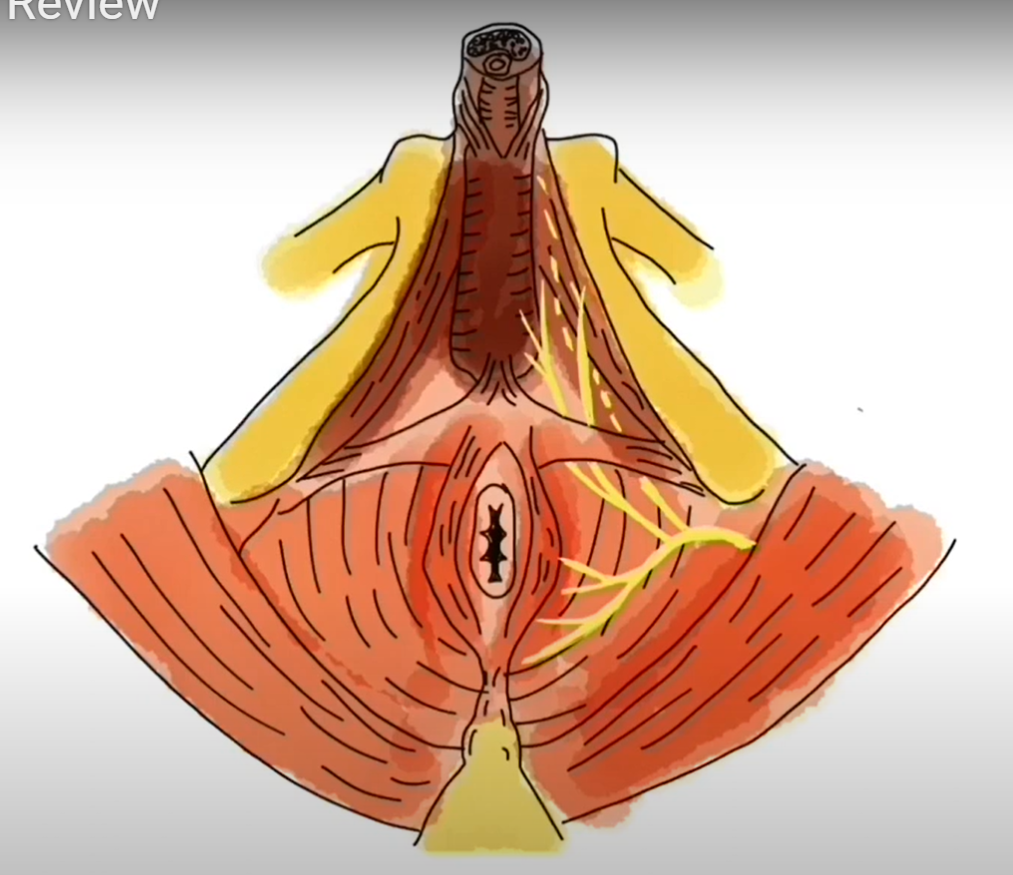
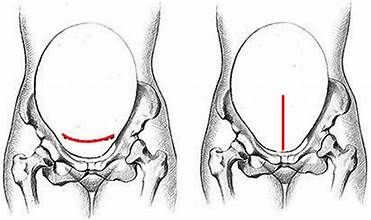
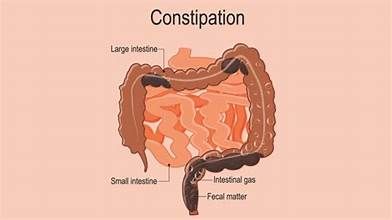
In this picture, you can see the colon/rectum directly in front of the tailbone. Surrounding the rectum like a small ring are your pelvic floor muscles. When these muscles are relaxed, your rectum and rectal canal are at the perfect angle to allow stool to pass through. However, if these muscles are not relaxing this can put a “kink in the hose” so to speak. This changes the angle of the rectum and can make it difficult for anything to pass through.This is where your PT can help. He or she will be equipped to assess the muscles of your pelvic floor for strength and coordination, and give you many tips and tricks to make bowel movements easier. Here are a few things your therapist might suggest:
Bowel Do’s:
Be sure you’re getting enough water and fiber
Initiate a bowel routine
Elevate your feet using a stool or Squatty Potty when sitting on the toilet -- see video link below
Get 10-20 minutes of exercise daily
Inhale, then exhale as you try to empty the stool
Look before you flush - thin pencil like stool or round hard pellets are not normal. See link to Bristol Stool chart, Type 4 is ideal⁷
Dont's:
Strain to have a bowel movement
Restrict food intake
Sit on the toilet with your hips higher than your knees
Maintain a sedentary lifestyle
Hold your breath while having a bowel movement
Empty your bowels in a hurry. Find a good bathroom read and take your time!
The gut is a complex system. If you are struggling with constipation, talk to your provider about treatment options. A pelvic floor physical therapist can be a great addition to your medical team, and can give you unique insight on how to move towards complete bowel health.
- www.ucsfhealth.org/increasing_fiber_intake. University of California San Francisco Medical Center.
- Institute of Medicine. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Institute of Medicine Panel on Dietary Reference Intakes for Electrolytes and Water, Standing Committee on the Scientific Evaluation of Dietary Reference Intakes Washington, D.C. National Academies Press 2005.
- Mitsuhasi et al. Characterizing Normal Bowel Frequency and Consistency in a Representative Sample of Adults in the United States. American Journal of Gastroenterology. May 2017
- Shih D M.D. and Kwan L M.D. All Roads Lead to Rome: Update on Rome III Criteria and New Treatment Options. Gastroenterol Rep. 2007 Winter
- Heymen S, Scarlett Y, Jones K et al. Randomized, controlled trial shows biofeedback to be superior to alternative treatments for patients with pelvic floor dyssynergia-type. Dis Colon Rectum. 2007 Apr; 50(4):428-41.
- http://www.pelvicexercises.com. How to Empty Your Bowels to Overcome Bowel Movement Problems.
- https://www.continence.org.au/pages/bristol-stool-chart.html. Bristol Stool Chart